Содержание
- 2. Thyroid cancers ~1% of new cancer diagnoses in the USA each year the incidence is 3
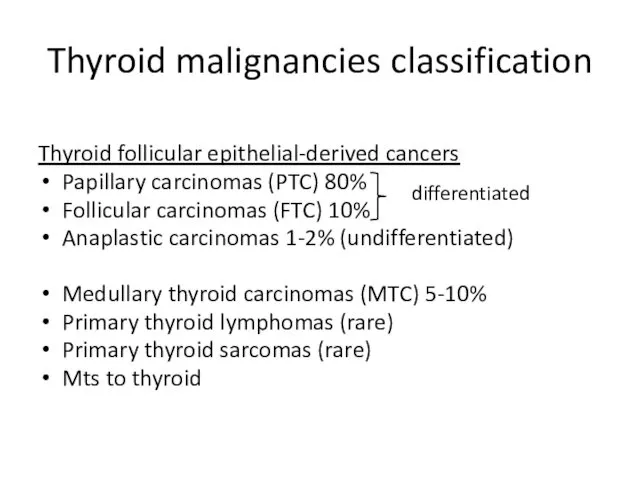
- 3. Thyroid malignancies classification Thyroid follicular epithelial-derived cancers Papillary carcinomas (PTC) 80% Follicular carcinomas (FTC) 10% Anaplastic
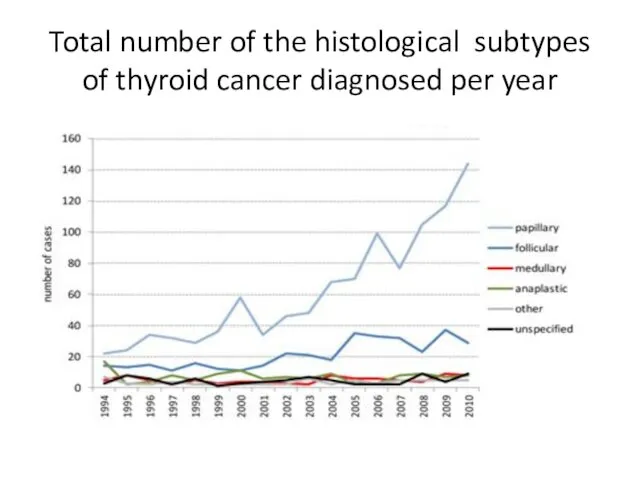
- 4. Total number of the histological subtypes of thyroid cancer diagnosed per year
- 5. Clinical picture of thyroid cancer painless, palpable, solitary thyroid nodule ~4-7% of the general population on
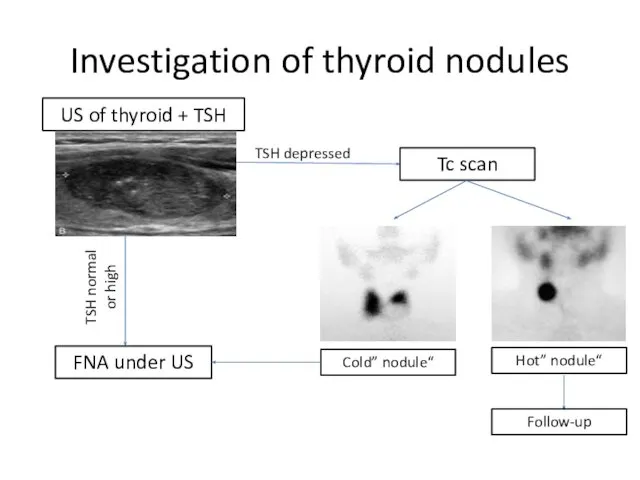
- 6. Investigation of thyroid nodules US of thyroid + TSH TSH depressed TSH normal or high FNA
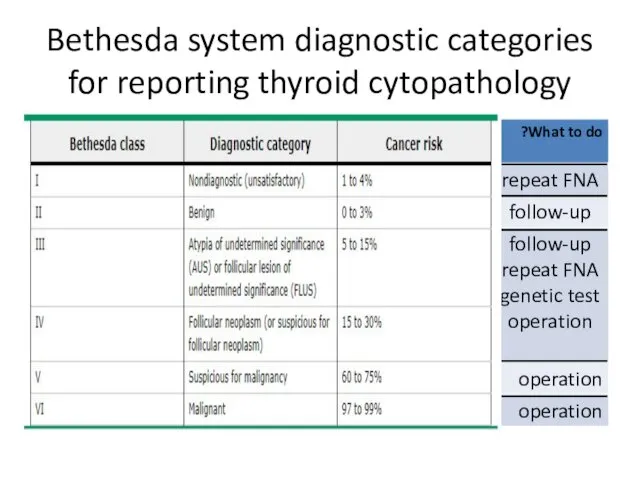
- 7. Bethesda system diagnostic categories for reporting thyroid cytopathology
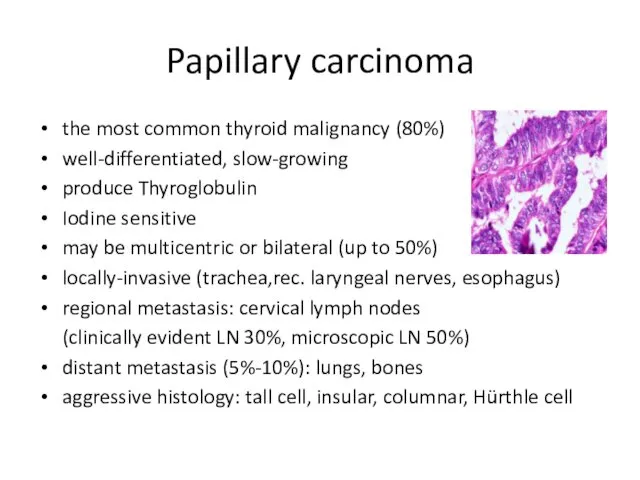
- 8. Papillary carcinoma the most common thyroid malignancy (80%) well-differentiated, slow-growing produce Thyroglobulin Iodine sensitive may be
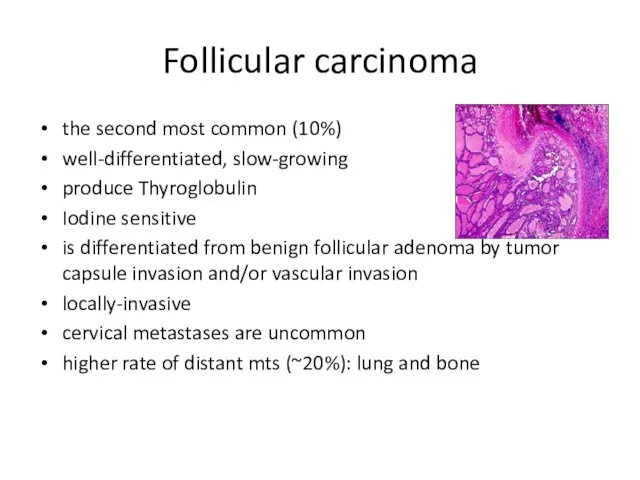
- 9. Follicular carcinoma the second most common (10%) well-differentiated, slow-growing produce Thyroglobulin Iodine sensitive is differentiated from
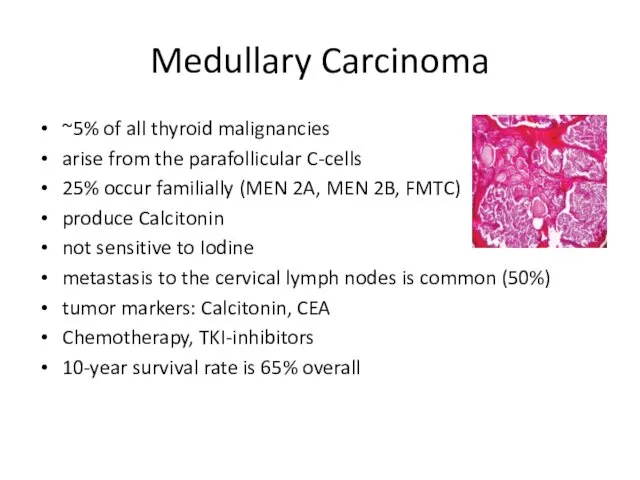
- 10. Medullary Carcinoma ~5% of all thyroid malignancies arise from the parafollicular C-cells 25% occur familially (MEN
- 11. Anaplastic Carcinoma one of the least common (~1.6%) most aggressive and one of the worst survival
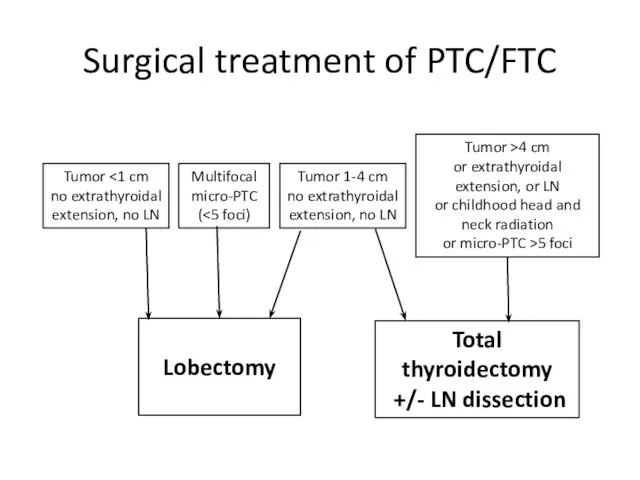
- 12. Surgical treatment of PTC/FTC Tumor no extrathyroidal extension, no LN Tumor 1-4 cm no extrathyroidal extension,
- 13. Complication of surgical treatment Hemorrhage Infection Reccurent laryngeal nerve injury (up to 10%) Bilateral vocal cord
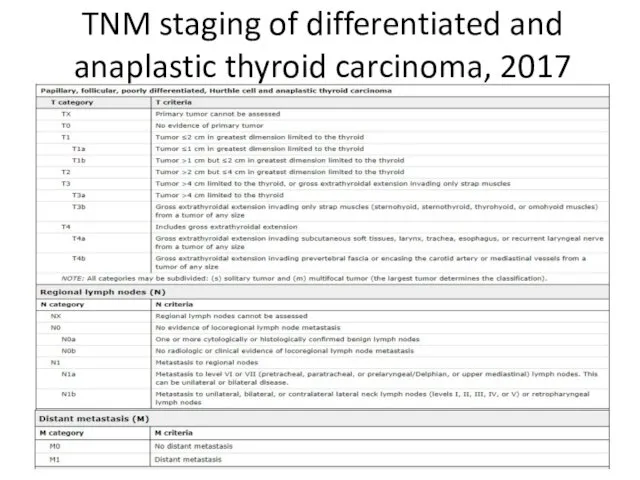
- 14. TNM staging of differentiated and anaplastic thyroid carcinoma, 2017
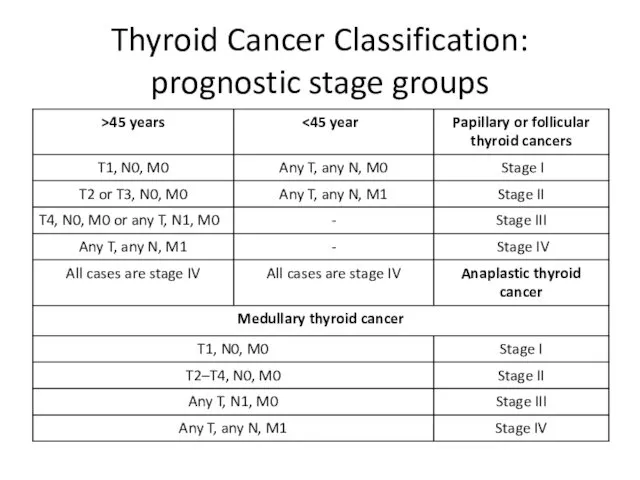
- 15. Thyroid Cancer Classification: prognostic stage groups
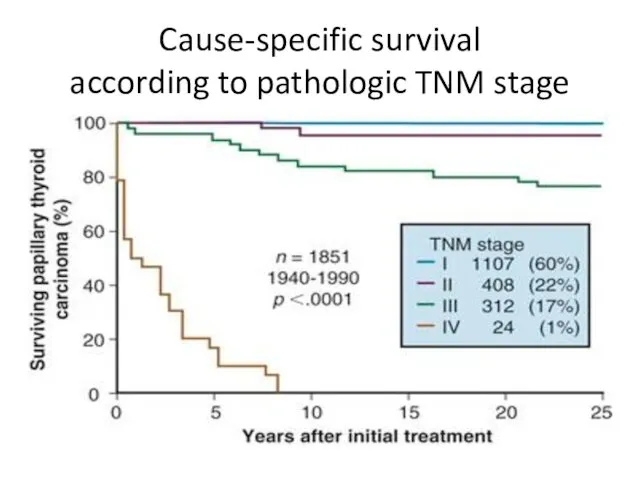
- 16. Cause-specific survival according to pathologic TNM stage
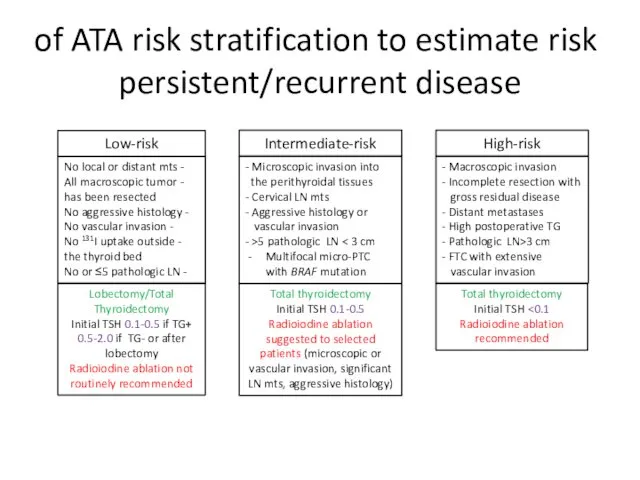
- 17. ATA risk stratification to estimate risk of persistent/recurrent disease Low-risk Intermediate-risk High-risk - No local or
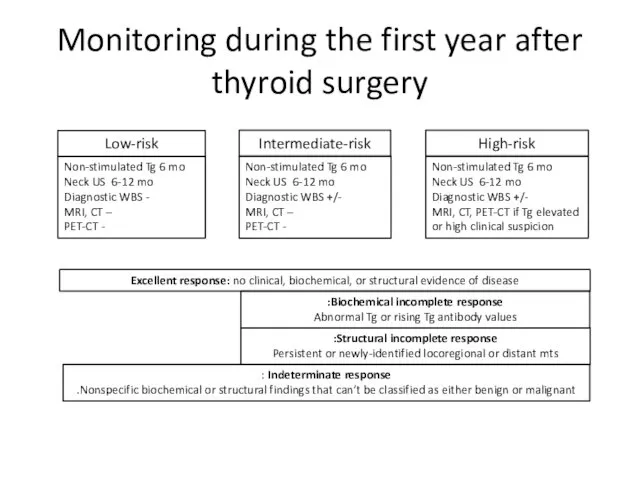
- 18. Monitoring during the first year after thyroid surgery Low-risk Intermediate-risk High-risk Non-stimulated Tg 6 mo Neck
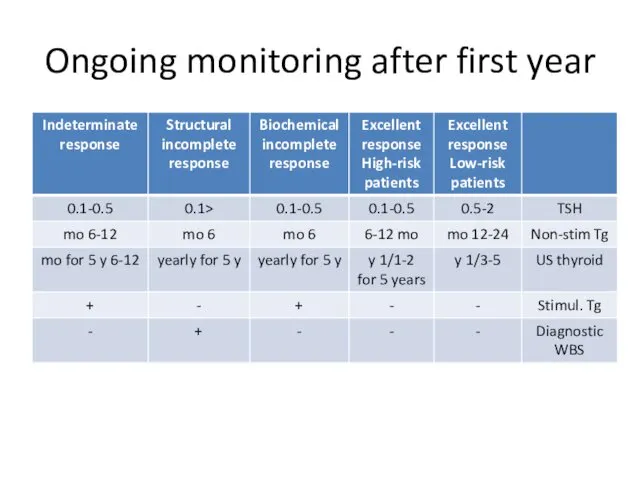
- 19. Ongoing monitoring after first year
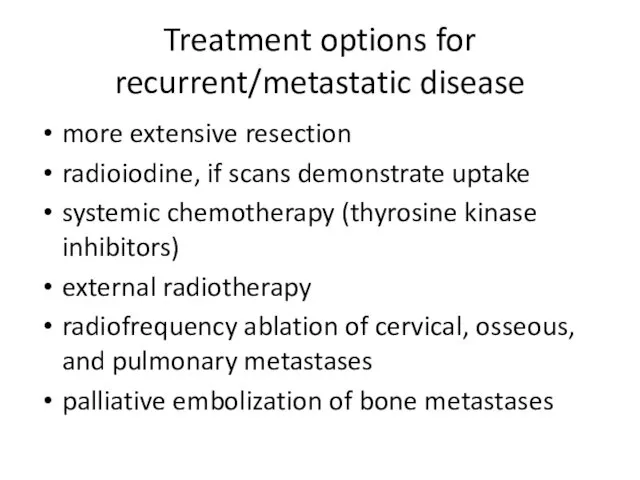
- 20. Treatment options for recurrent/metastatic disease more extensive resection radioiodine, if scans demonstrate uptake systemic chemotherapy (thyrosine
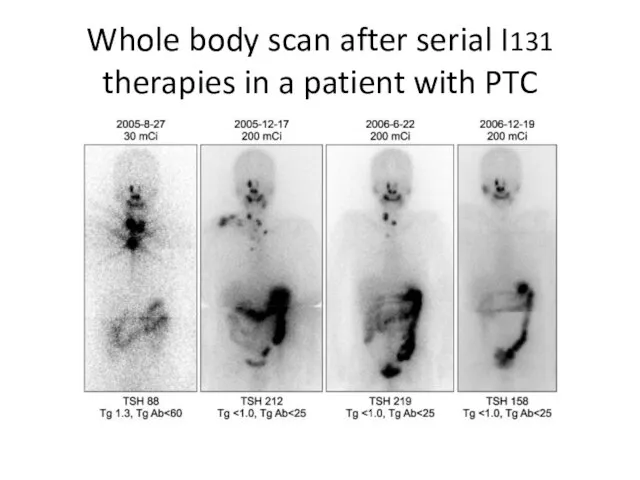
- 21. Whole body scan after serial I131 therapies in a patient with PTC
- 23. Скачать презентацию
 Ларингоспазм.Бронхоспазм.Бронх демікпесі
Ларингоспазм.Бронхоспазм.Бронх демікпесі Воспаление. Общие проявления воспаления
Воспаление. Общие проявления воспаления Примеры работ
Примеры работ Развитие речи в онтогенезе
Развитие речи в онтогенезе Реставрация костного препарата (черепа)
Реставрация костного препарата (черепа) Рекомендации по реваскуляризации миокарда (ESC 2018)
Рекомендации по реваскуляризации миокарда (ESC 2018) Раневая инфекция
Раневая инфекция Клиническая фармакология противовирусных средств
Клиническая фармакология противовирусных средств Для здорового баланса микрофлоры кишечника
Для здорового баланса микрофлоры кишечника Клименко
Клименко Оценка тяжести состояния. Триаж
Оценка тяжести состояния. Триаж Эксперименты на человеке
Эксперименты на человеке Адаптация к физическим упражнениям
Адаптация к физическим упражнениям Клиника родов. Лекция 1
Клиника родов. Лекция 1 Мембрано-пролиферативный гломерулонефрит
Мембрано-пролиферативный гломерулонефрит Проблема неконролируемого отпуска лекарственных средств по рецепту
Проблема неконролируемого отпуска лекарственных средств по рецепту Оптимизация терапии Helicobacter pylori-ассоциированной патологии верхних отделов желудочно-кишечного тракта у детей
Оптимизация терапии Helicobacter pylori-ассоциированной патологии верхних отделов желудочно-кишечного тракта у детей Сенсорные и гностические слуховые расстройства. Слуховые агнозии
Сенсорные и гностические слуховые расстройства. Слуховые агнозии Психология детей с нарушениями эмоциональноволевой сферы и поведения. Лекция 1
Психология детей с нарушениями эмоциональноволевой сферы и поведения. Лекция 1 Bronchial asthma
Bronchial asthma Проблемы пациента с пояснично-крестцовым радикулитом и реализация программы сестринских вмешательств
Проблемы пациента с пояснично-крестцовым радикулитом и реализация программы сестринских вмешательств Технология изотовления жидких лекарственных форм-суспензий
Технология изотовления жидких лекарственных форм-суспензий Кроветворение (гемопоэз)
Кроветворение (гемопоэз) Неонатальные желтухи
Неонатальные желтухи Паренхиматозды мүшелердің жабық жарақаты
Паренхиматозды мүшелердің жабық жарақаты Жалпы тәжірибелік дәрігер туралы түсінік
Жалпы тәжірибелік дәрігер туралы түсінік Когнитивные технологии в управлении человеческими ресурсами: стресс-менеджмент
Когнитивные технологии в управлении человеческими ресурсами: стресс-менеджмент Рентген аппарат
Рентген аппарат