Содержание
- 2. The Case Kali is a 14mo female who presents to WRAMC ED with fever to 102.
- 3. The Case Kali is a 14mo female who presents to WRAMC ED with fever to 102.
- 4. The Case Kali is a 14mo female who presents to WRAMC ED with fever to 102.
- 5. The Question Should we treat her prophylactically? Short-term: Will this decrease recurrent infections? Long-term: Will this
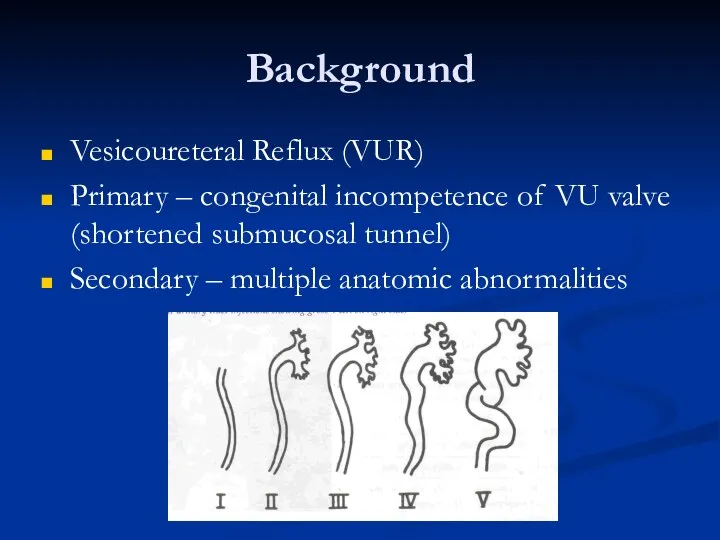
- 6. Background Vesicoureteral Reflux (VUR) Primary – congenital incompetence of VU valve (shortened submucosal tunnel) Secondary –
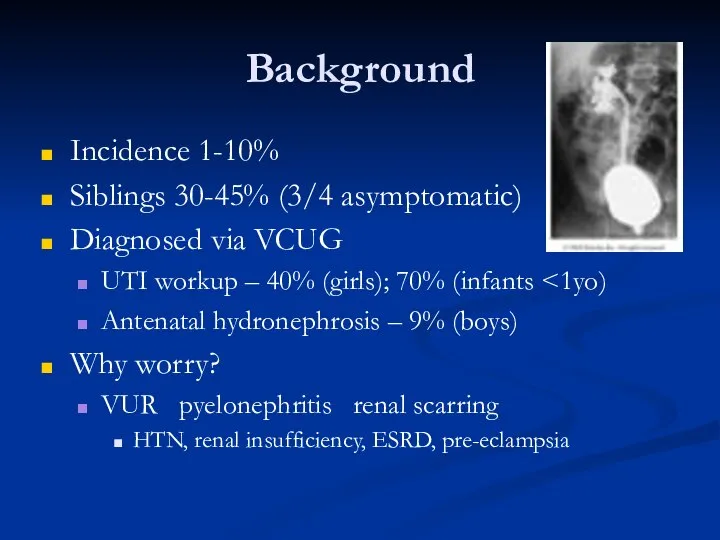
- 7. Background Incidence 1-10% Siblings 30-45% (3/4 asymptomatic) Diagnosed via VCUG UTI workup – 40% (girls); 70%
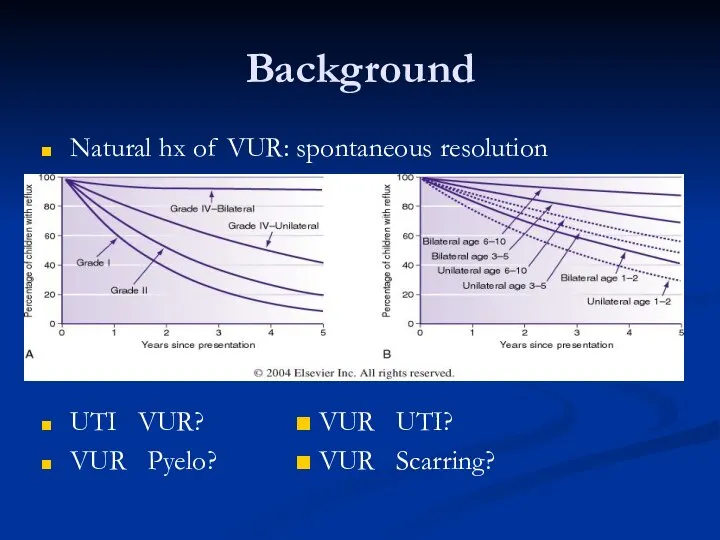
- 8. Background Natural hx of VUR: spontaneous resolution UTI ? VUR? ■ VUR ? UTI? VUR ?
- 9. Current Treatment Recs Workup: Febrile UTI (any age) UTI UTI x2 in school-age girls UTI in
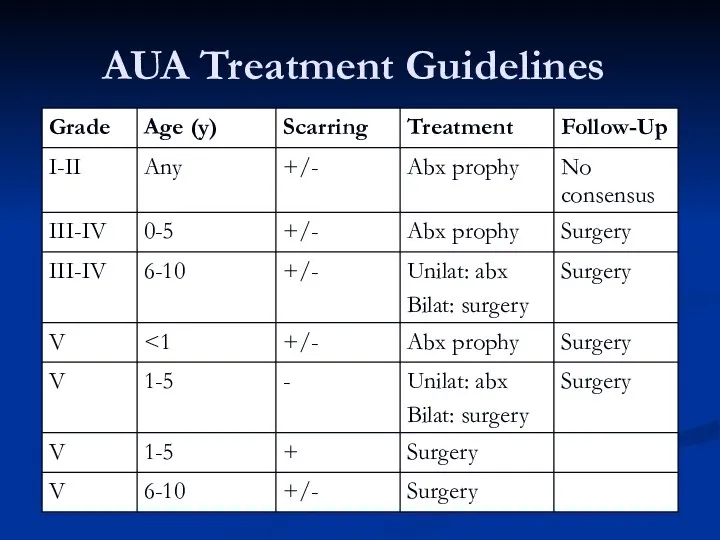
- 10. AUA Treatment Guidelines
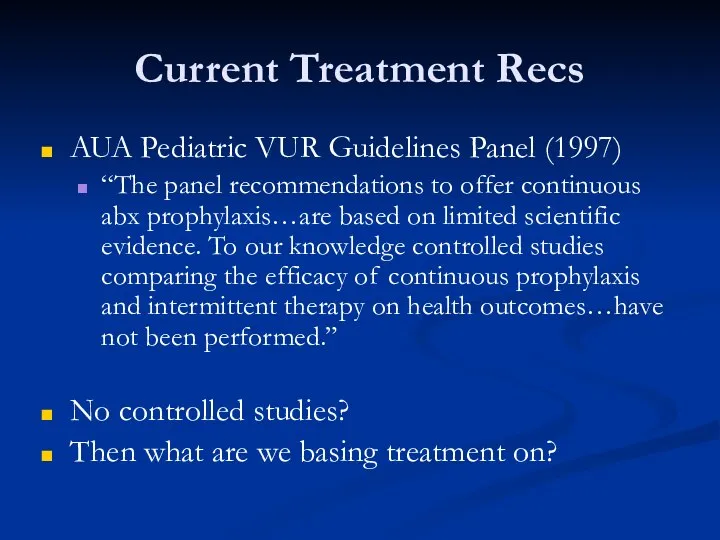
- 11. Current Treatment Recs AUA Pediatric VUR Guidelines Panel (1997) “The panel recommendations to offer continuous abx
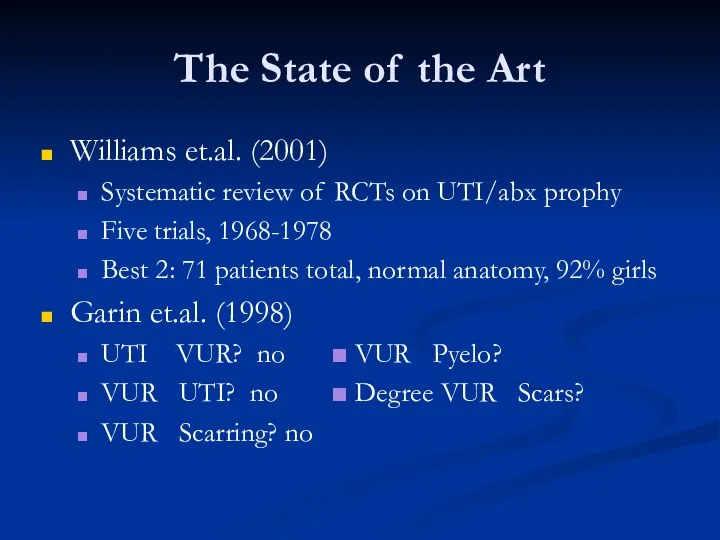
- 12. The State of the Art Williams et.al. (2001) Systematic review of RCTs on UTI/abx prophy Five
- 13. We Need A Study That… Will help us decide whether or not to prophylax this patient
- 14. Clinical significance of primary vesicoureteral reflux and urinary antibiotic prophylaxis after acute pyelonephritis: a multicenter, randomized,
- 15. Study Questions Does VUR correlate with ?UTI/renal scarring? Does antibiotic prophylaxis correlate with ?UTI/renal scarring?
- 16. Study Design Randomized, controlled, multicenter trial Inclusion: 3mo-18yo Acute pyelonephritis Exclusion: Grade IV-V VUR Anatomic abnormalities
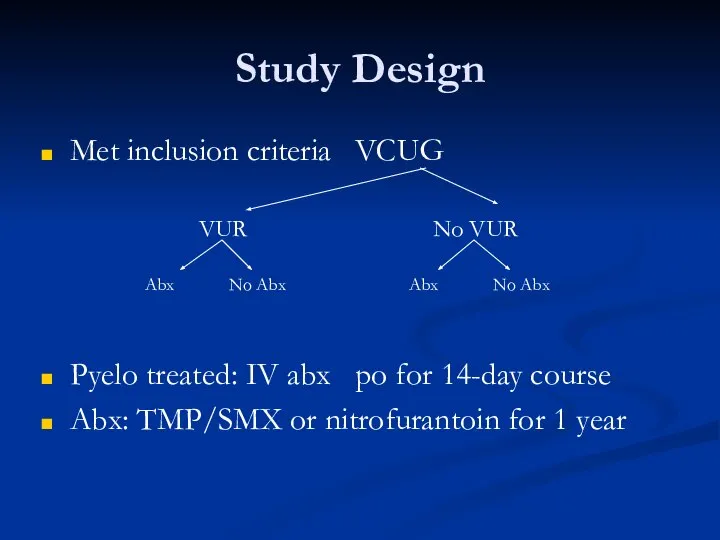
- 17. Study Design Met inclusion criteria ? VCUG Pyelo treated: IV abx ? po for 14-day course
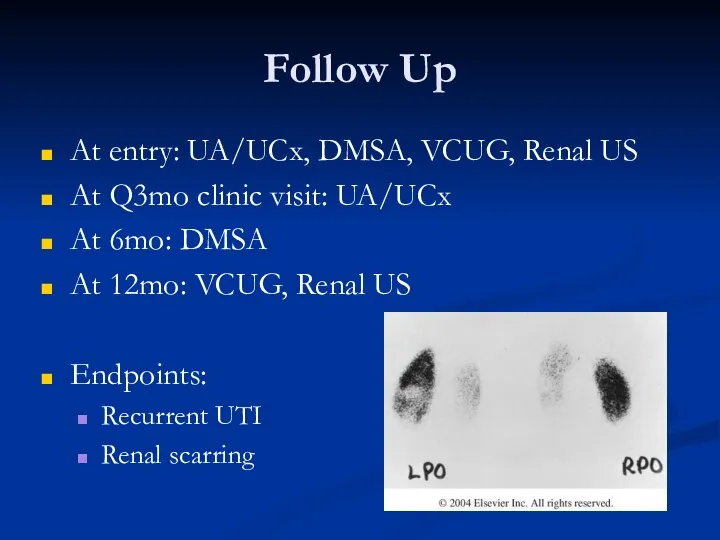
- 18. Follow Up At entry: UA/UCx, DMSA, VCUG, Renal US At Q3mo clinic visit: UA/UCx At 6mo:
- 19. Study Results
- 20. Analysis of Results Fisher’s Exact Test 2x2 comparison tables Control vs. variable Smaller sample size Gives
- 21. Study Results Recurrence of UTIs Timing Type Recurrent Pyelonephritis & Antibiotics Recurrent Pyelonephritis & VUR Degree
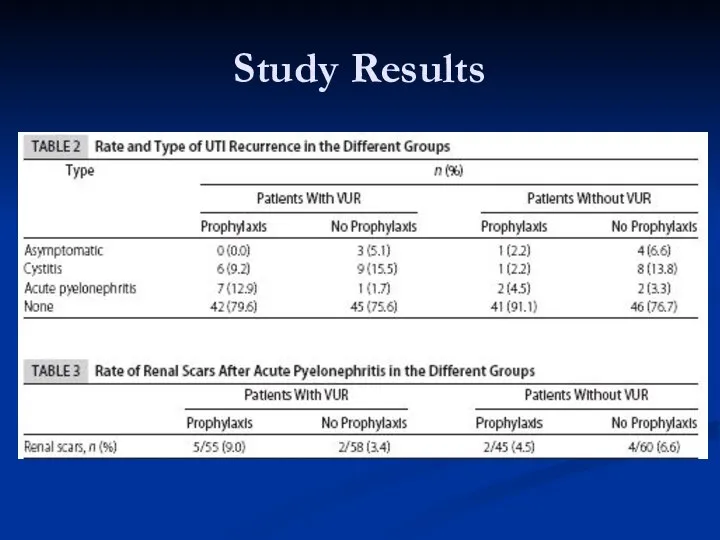
- 22. Study Results Recurrence of UTI Overall – 20.1% VUR not significant No abx (p=.9999) VUR –
- 23. Study Results Recurrent Pyelo and Antibiotics No benefit of abx (p=.0291) 7:1 abx:none Recurrent Pyelo and
- 24. Study Results Renal Scarring No evidence VUR? increased scarring (p=.9999) VUR (6.2%) = No VUR (5.7%)
- 25. Study Conclusions Mild/moderate VUR not associated with ?UTI, pyelonephritis, or scarring Antibiotic prophylaxis not associated with
- 26. Critically Evaluating… (JAMA Users’ Guide) Are the results valid? What were the results? Will the results
- 27. Are the results valid? Primary Guides Was the assignment of patients to treatment randomized? YES. Were
- 28. Are the results valid? Secondary Guides Were pts, clinicians, & study personnel blinded? NO (no blinding
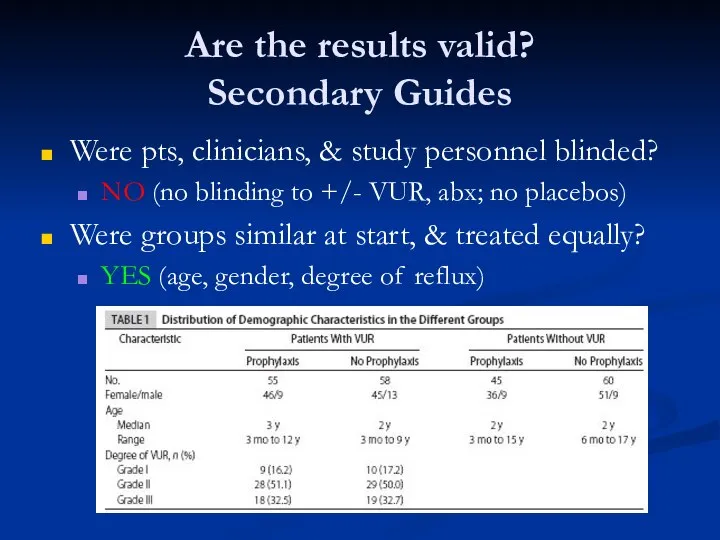
- 29. What were the results? How large was the treatment effect? ARR – risk difference of variable
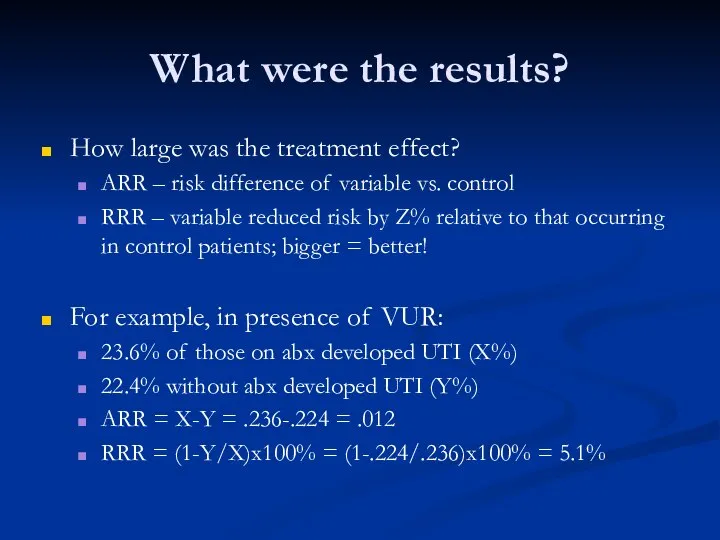
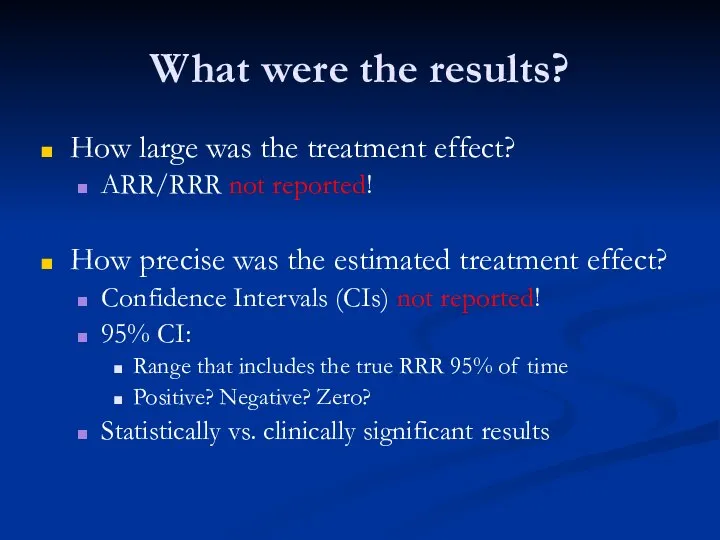
- 30. What were the results? How large was the treatment effect? ARR/RRR not reported! How precise was
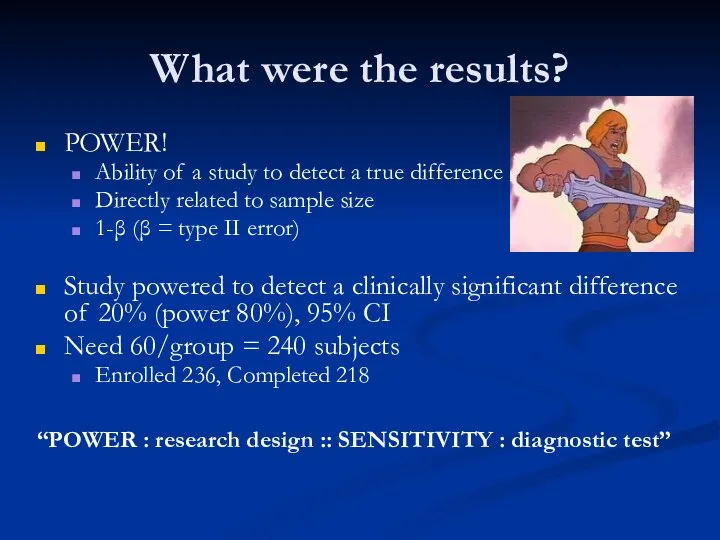
- 31. What were the results? POWER! Ability of a study to detect a true difference Directly related
- 32. Will the results help me take care of my patient? Can the results be applied? YES.
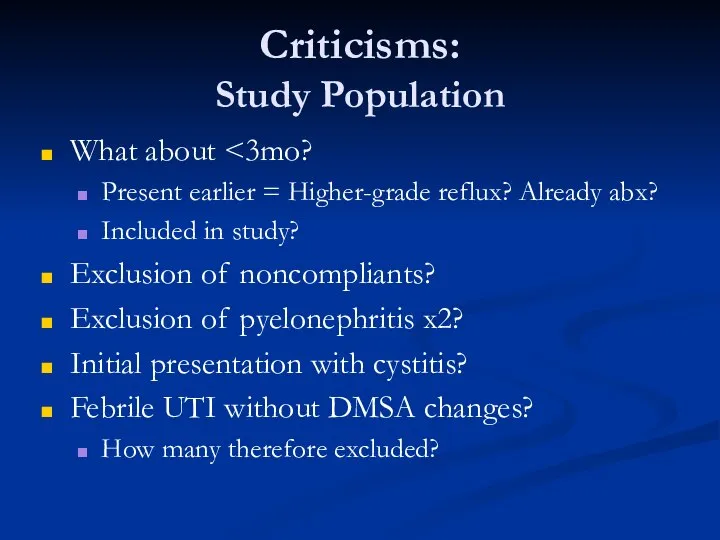
- 33. Criticisms: Study Population What about Present earlier = Higher-grade reflux? Already abx? Included in study? Exclusion
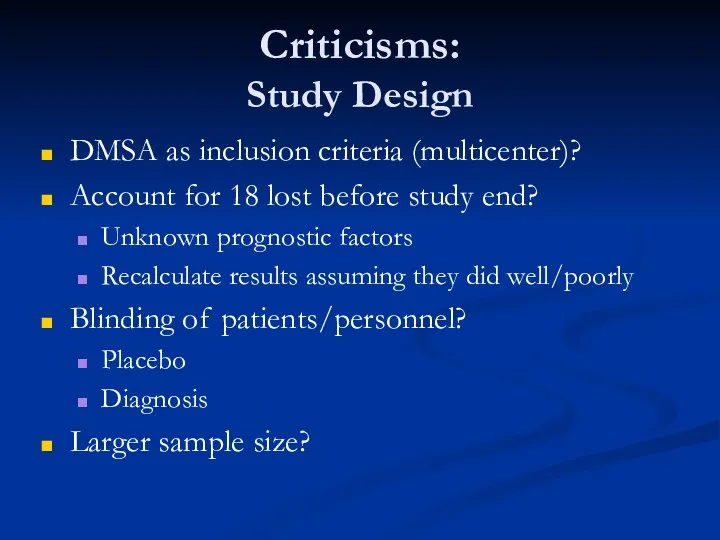
- 34. Criticisms: Study Design DMSA as inclusion criteria (multicenter)? Account for 18 lost before study end? Unknown
- 35. Criticisms: Data Analysis Reporting of CIs, ARR/RRR? Magnitude/precision of treatment effect Rule in/out effect different from
- 36. Further Questions… UTI prophylaxis vs. intermittent therapy? And risk of renal scarring Over time, given resolution
- 37. Back to our patient… What would you do? Call Dr.Cartwright and Dr.Lechner and get those patients
- 38. References Atala A, Keating MA. Vesicoureteral reflux and megaureter. In Campbell’s Urology Vol 2, 7th ed.
- 40. Скачать презентацию











 Спленэктомия. Техникасы
Спленэктомия. Техникасы Танымдық психикалық процестер: түйсік, қабылдау
Танымдық психикалық процестер: түйсік, қабылдау Рак яичника
Рак яичника Сбор и сушка растительного сырья. Оформление гербария. Тема 1.9
Сбор и сушка растительного сырья. Оформление гербария. Тема 1.9 Вегетативная нервная система. Методы обследования в неврологии. (Занятие 8)
Вегетативная нервная система. Методы обследования в неврологии. (Занятие 8) Диагностика и лечение варикозной болезни вен нижних конечностей
Диагностика и лечение варикозной болезни вен нижних конечностей Анатомо-физиологические особенности строения полости рта в возрастном аспекте
Анатомо-физиологические особенности строения полости рта в возрастном аспекте Беременность и ВПЧ-инфекция
Беременность и ВПЧ-инфекция Чувства, эмоции
Чувства, эмоции Проект Бережливая поликлиника
Проект Бережливая поликлиника Ведение беременности и родов при туберкулёзе
Ведение беременности и родов при туберкулёзе Изучение причин возникновения и профилактика пищевых отравлений и инфекционных заболеваний
Изучение причин возникновения и профилактика пищевых отравлений и инфекционных заболеваний Массовые истерии
Массовые истерии Систематические обзоры и мета-анализ статей
Систематические обзоры и мета-анализ статей Первичные бактериальные менингиты. Диагностика и лечение
Первичные бактериальные менингиты. Диагностика и лечение Пухлини органів травлення
Пухлини органів травлення Научно-исследовательская работа: Шумовые загрязнения влияющие на здоровье человека.
Научно-исследовательская работа: Шумовые загрязнения влияющие на здоровье человека. Резиденттің өзіндік жұмысы
Резиденттің өзіндік жұмысы Основы эргономики и безопасности перемещения пациента
Основы эргономики и безопасности перемещения пациента Массаж. Илеу
Массаж. Илеу Basic life support
Basic life support Міопатії. Невральні аміотрофії. Міотонія Томпсона
Міопатії. Невральні аміотрофії. Міотонія Томпсона Общая рецептура твердые и мягкие лекарственные формы/ /жидкие лекарственные формы
Общая рецептура твердые и мягкие лекарственные формы/ /жидкие лекарственные формы Морфологические и физиологические особенности плода в разные периоды внутриутробного развития
Морфологические и физиологические особенности плода в разные периоды внутриутробного развития Внимание и воля
Внимание и воля Медицина эпохи Возрождения
Медицина эпохи Возрождения Лекарственные растения и лекарственное сырье, применяемое при лечении и профилактики атеросклероза
Лекарственные растения и лекарственное сырье, применяемое при лечении и профилактики атеросклероза Аллергия - проблема XXI века
Аллергия - проблема XXI века