Maximizing the medical treatment of endometriosis, the double progestin system (DPS) for difficult endometriosis
Содержание
- 2. Declaration I declare no conflict of interests
- 3. Notion Medical treatment should be the first line modality for Deep Endometriosis (DE) in women with
- 4. Facts No medical therapy is effective on all patients with a chronic condition; Effective drugs with
- 5. Current status regarding surgical Rx for DE For almost a century, the surgical treatment of endometriosis
- 6. Population-based data do not suggest that conservative surgery constitutes a durable remedy for severely symptomatic endometriosis
- 7. Recurrence of deep lesions after surgery A repeat procedure within 5 years from primary surgery because
- 8. Recurrence after surgery NICE Committee maintained “in view of the high rate of recurrence of endometriosis,
- 9. Impact of endometriosis on risk of further gynaecological surgery: a national cohort study The incidence of
- 10. Complications of surgery for DE The overall complication rate was 24%, and the severe complication rate
- 11. A- De Cicco C, Corona R, Schonman R, Mailova K, Ussia A, Koninckx P. Bowel resection
- 12. So what advice could we sensibly give women who need to decide on whether they opt
- 13. Medical rx for endometriosis
- 14. Medical treatment for DE (Andres,MP, 2019) Methods: Retrospective study based on data extracted from medical records
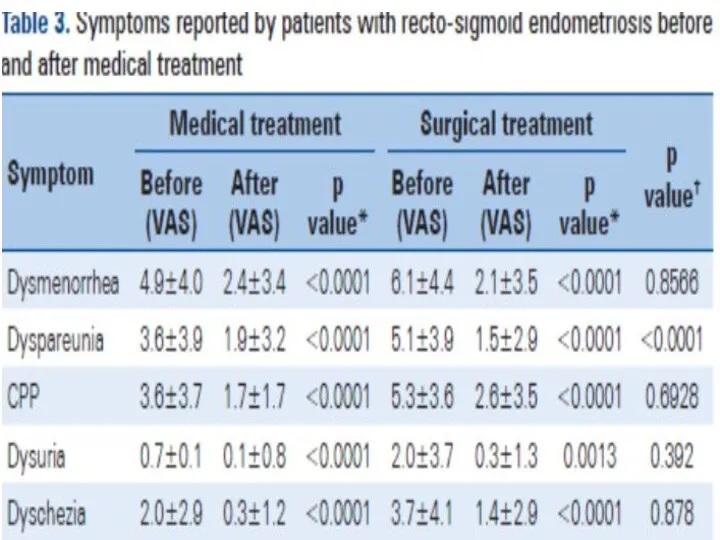
- 18. Symptom progression in patients with recto-sigmoid endometriosis submitted to medical or surgical treatment
- 19. Factors to be considered before treatment plan decision for DE Severity of symptoms Size of the
- 20. A lesion-based, three-tiered risk stratification system a. Low-risk lesion: superficial peritoneal implants- progressed in only one
- 21. A symptom-based, stepped-care approach NICE Committee confirmed two fundamental principles (1): (1) “all treatments led to
- 22. A symptom-based, stepped-care approach low-dose OCs should be used cyclically in women with peritoneal and ovarian
- 23. The goal of endometriosis therapy “the goal of endometriosis therapy should always be absence of pain;
- 24. The burden of illness and the burden of treatment The burden of illness: Women with severely
- 25. Pros and cons of combined oral contraceptives In a large, multicenter, placebo-controlled RCT conducted in women
- 26. Use of OCs continuously instead of cyclically!! When pooling published data, no statistically significant differences were
- 27. Pros and cons of progestogens Hormonal activities of progestogens investigated for the treatment of endometriosis. Literature
- 28. Cost of progestogens Low-cost progestogens include medroxyprogesterone acetate (MAP), norethisterone acetate (NETA), levonorgestrel (LNG), and nomegestrol
- 29. “Every woman is unique and so is her response to progestogen, hence, we need to explore
- 30. GnRH agonists The profound hypoestrogenic state achieved during the use of these drugs explains their efficacy
- 31. GnRH antagonist-Elagolix, The GnRH antagonist at the oral daily dose of 150 or 400 mg was
- 32. Dual progestogen-delivery system (DPS) therapy with levonorgestrel intrauterine system and etonogestrel subdermal implant for severe and
- 34. DPS (Dual progestogen-delivery System) for refractory endometriosis Objective: To explore the usefulness of simultaneous use of
- 35. Women refractory to conventional therapies Management of endometriosis depends primarily on whether the woman wishes to
- 36. LNG-IUS & etonogestrel subdermal implant for endometriosis Recently, there has been a gradual move towards greater
- 37. Rational for combination When both systems are combined a steady low-dose delivery of progestogens is maintained
- 38. Ethics approval & Indications for the combined therapy This retrospective case series was approved by the
- 39. DPS Objective: To explore the usefulness of simultaneous use of dual progestogen-delivery systems (DPS) with the
- 40. Results: The mean duration of use of the DPS was 28.1 (range 9 – 98) months.
- 41. Conclusions: The combination DPS appears to be an effective new medical option in management of refractory
- 43. Скачать презентацию

























 Бронхиальная астма в условиях терапевтического участка
Бронхиальная астма в условиях терапевтического участка Питание во время химиотерапии
Питание во время химиотерапии Боль в спине и шее
Боль в спине и шее Новая классификация эпилептических приступов и эпилепсий. Разбор клинического случая
Новая классификация эпилептических приступов и эпилепсий. Разбор клинического случая Чинники, що визначають привабливість дівчини для студентів НаУКМА
Чинники, що визначають привабливість дівчини для студентів НаУКМА Мүмкіндіктері шектеулі науқастармен қарым-қатынас
Мүмкіндіктері шектеулі науқастармен қарым-қатынас Физиология коры больших полушарий. Основы физиологии поведения и научения
Физиология коры больших полушарий. Основы физиологии поведения и научения Экспертиза временной нетрудоспособности работника
Экспертиза временной нетрудоспособности работника Психология личности. Сестринское дело. Переподготовка
Психология личности. Сестринское дело. Переподготовка Действие ферментов желудочного сока на белки
Действие ферментов желудочного сока на белки Оценка скрининговых осмотров. Индикаторы оценки
Оценка скрининговых осмотров. Индикаторы оценки Фарингоскопия
Фарингоскопия Генетические основы опухолевого роста Патоморфологические особенности опухолей
Генетические основы опухолевого роста Патоморфологические особенности опухолей Здоровое питание школьников
Здоровое питание школьников Новая коронавирусная инфекция
Новая коронавирусная инфекция Тучность. Метаболический синдром
Тучность. Метаболический синдром Патология пищеварительной системы
Патология пищеварительной системы Дежурства спасателей экипажа Красного Креста
Дежурства спасателей экипажа Красного Креста Развитие органов дыхательной системы
Развитие органов дыхательной системы Лечение наркомании
Лечение наркомании Внимание и память
Внимание и память Балалардың асқазан - ішек аурулары туралы түсінік беру. Балаларда ішек жұқпасының көріністері
Балалардың асқазан - ішек аурулары туралы түсінік беру. Балаларда ішек жұқпасының көріністері Хроническая почечная недостаточность (ХПН)
Хроническая почечная недостаточность (ХПН) Острая сердечная недостаточность
Острая сердечная недостаточность Методы формирования бесконфликтного общения у младших школьников
Методы формирования бесконфликтного общения у младших школьников Нарушения голоса
Нарушения голоса Острые кишечные заболевания
Острые кишечные заболевания Методы машинной обработки корневых каналов
Методы машинной обработки корневых каналов