Содержание
- 2. Primary Secondary
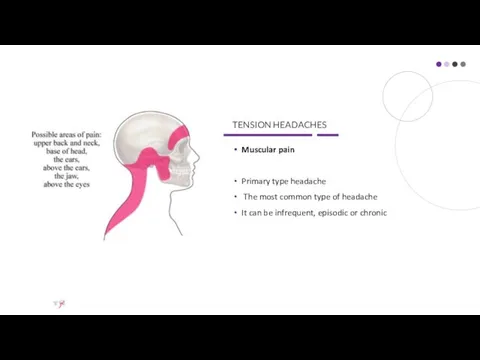
- 3. TENSION HEADACHES Muscular pain Primary type headache The most common type of headache It can be
- 4. Simptoms dull ache, like a ‘tight pressure feeling’, ‘heavy weight almost daily hours (can last days)
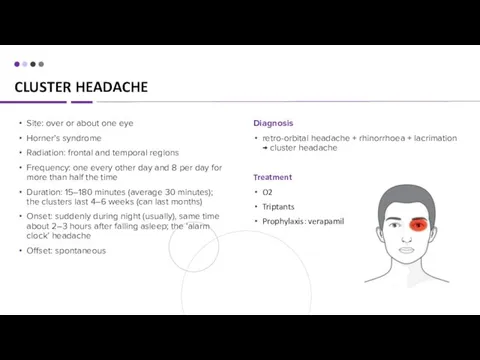
- 5. CLUSTER HEADACHE Diagnosis retro-orbital headache + rhinorrhoea + lacrimation → cluster headache Treatment O2 Triptants Prophylaxis:
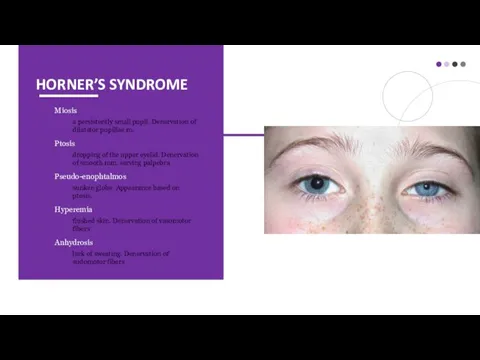
- 6. HORNER’S SYNDROME Miosis a persistently small pupil. Denervation of dilatator pupillae m. Ptosis dropping of the
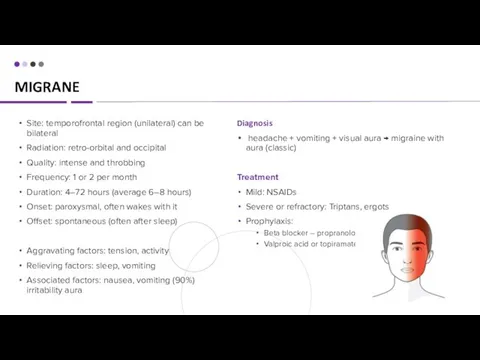
- 7. MIGRANE Diagnosis headache + vomiting + visual aura → migraine with aura (classic) Treatment Mild: NSAIDs
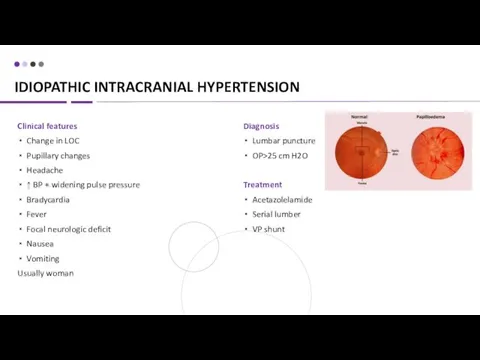
- 8. IDIOPATHIC INTRACRANIAL HYPERTENSION Clinical features Change in LOC Pupillary changes Headache ↑ BP + widening pulse
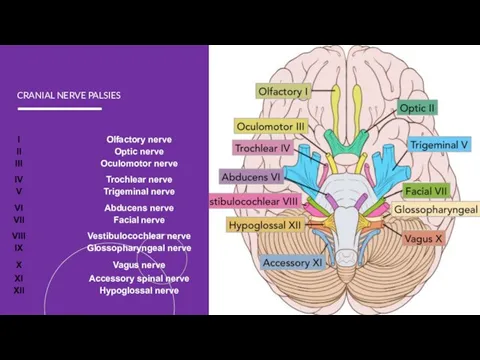
- 9. CRANIAL NERVE PALSIES
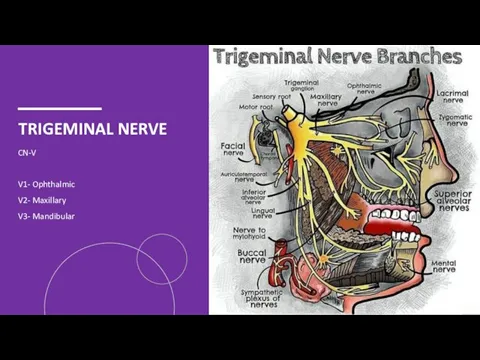
- 10. TRIGEMINAL NERVE CN-V V1- Ophthalmic V2- Maxillary V3- Mandibular
- 11. TRIGEMINAL NEURALGIA Causes Idiopathic or compression of the TN Local pressure on the nerve root entry
- 12. TRIGEMINAL NEURALGIA Treatment Carbamazepine Oxcarbazepine Baclofen Lamotrigine Surgical Diagnosis Clx MRI to rule out secondary causes
- 13. FACIAL NERVE CN – 7 frontal (or temporal) zygomatic buccal marginal mandibular cervical
- 14. BELL’S PALSY Causes infection or inflammation of the facial nerve head trauma head or neck tumor
- 15. BELL’S PALSY Treatment Supportive: Artificial tears if eye is dry and at bedtime Massage and facial
- 16. LUMBAR PUNCTURE Preparing Stop taking blood-thinning medications, such as aspirin and warfarin. Tell your doctor if
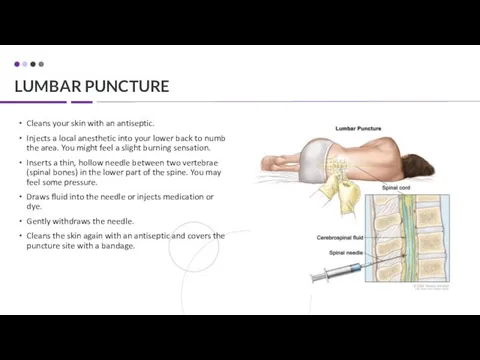
- 17. LUMBAR PUNCTURE Cleans your skin with an antiseptic. Injects a local anesthetic into your lower back
- 19. DISORDERS OF THE VISUAL PATHWAY
- 20. APPROACH TO SYNCOPE
- 21. APPROACH TO SYNCOPE W vasovagal Visceral Baroreceptors Psychogenic Situational and recurrent Drop 50 points in the
- 22. APPROACH TO SYNCOPE Orthostatic hypotension Volume down: dehydration, diarrhea, diaresis and hemorrhage Dysfunctional autonomic nervous system:
- 23. APPROACH TO SYNCOPE Psych Dx: face-palm maneuver Electrolytes Dx: BMP Na, Ca – mental status K,
- 26. Скачать презентацию












 Типы высшей нервной деятельности
Типы высшей нервной деятельности Лечебные грязи Крыма
Лечебные грязи Крыма Мероприятия по снижению распространения злокачественных новообразований среди женщин в Свердловской области
Мероприятия по снижению распространения злокачественных новообразований среди женщин в Свердловской области Набор в детский оздоровительный санаторий в г. Евпатория для детей от 10 до 14 лет,
Набор в детский оздоровительный санаторий в г. Евпатория для детей от 10 до 14 лет, № 2 Симптомдық артериальды гипертензия. № 3 вариант: Иценко-Кушинг синдромы кезіндегі
№ 2 Симптомдық артериальды гипертензия. № 3 вариант: Иценко-Кушинг синдромы кезіндегі Нервные и психические болезни
Нервные и психические болезни Оздоровчі системи
Оздоровчі системи Влияние анатомо-физиологических особенностей челюстно-лицевой области на клиническое течение воспалительных заболеваний
Влияние анатомо-физиологических особенностей челюстно-лицевой области на клиническое течение воспалительных заболеваний Клиническая фармакология препаратов, влияющих на функцию пищеварительной системы
Клиническая фармакология препаратов, влияющих на функцию пищеварительной системы Применение лекарственных средств
Применение лекарственных средств Рентгенодиагностика острой пневмонии у детей
Рентгенодиагностика острой пневмонии у детей Гипертоническая болезнь II стадии. Ситуационная задача
Гипертоническая болезнь II стадии. Ситуационная задача Патологическая анатомия ДВС-синдрома
Патологическая анатомия ДВС-синдрома Принципы неотложной помощи при судорожных припадках с потерей сознания
Принципы неотложной помощи при судорожных припадках с потерей сознания Составление проекта нормативной документации на лекарственные формы для парентерального введения
Составление проекта нормативной документации на лекарственные формы для парентерального введения Роль фельдшера в диагностике, лечении и профилактике закрытой черепно-мозговой травмы
Роль фельдшера в диагностике, лечении и профилактике закрытой черепно-мозговой травмы Врожденная косолапость
Врожденная косолапость Тиреотоксикалық криз және тиреотоксикалық кома
Тиреотоксикалық криз және тиреотоксикалық кома Хроническая болезнь почек при сахаром диабете
Хроническая болезнь почек при сахаром диабете Патофизиология обмена веществ
Патофизиология обмена веществ Скарлатина у детей дошкольного возраста
Скарлатина у детей дошкольного возраста Тиреотоксикалық криз және тиреотоксикалық кома
Тиреотоксикалық криз және тиреотоксикалық кома Пищевые токсикоинфекции
Пищевые токсикоинфекции Характер человека
Характер человека Поведенческие особенности и социализация в младенчестве
Поведенческие особенности и социализация в младенчестве Здоровый образ жизни – залог успешности специалиста
Здоровый образ жизни – залог успешности специалиста Духовные и физические аспекты эпилепсии
Духовные и физические аспекты эпилепсии Возрастная физиология (физиологические особенности детей и подростков)
Возрастная физиология (физиологические особенности детей и подростков)