Содержание
- 2. Disclosures None
- 3. Objectives Identify the neurogenic and mechanical factors which contribute to HSP Prescribe appropriate treatments for the
- 4. Outline Basics Definition, Incidence, Prognosis Anatomy Factors Neurogenic Mechanical Diagnosis Management Suggested Treatment Algorithm
- 5. Basics CVA: 795,000 per year; 3rd for mortality, 1st for disability; costs $18.8 billion annually Hemiplegia:
- 6. HSP Risk Factors Impaired motor control Diminished proprioception Tactile extinction Abnormal sensation Elbow flexor spasticity Restricted
- 7. HSP Prognosis Lower Barthel score at 12 weeks Lower chance of return home Resolution within first
- 8. Anatomy Shoulder: complex ball-and-socket joint Agility at the cost of stability Static stabilizers Glenohumeral ligaments Dynamic
- 9. Mechanisms of Injury Cause is likely multifactorial Weakness, spasticity, sensory loss, instability Classification Better by etiology
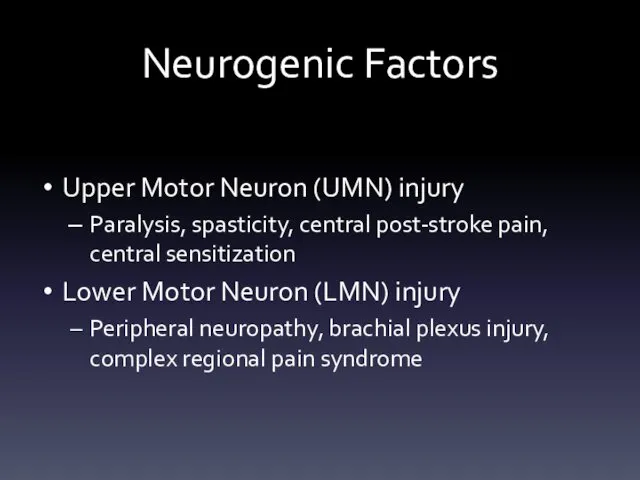
- 10. Neurogenic Factors Upper Motor Neuron (UMN) injury Paralysis, spasticity, central post-stroke pain, central sensitization Lower Motor
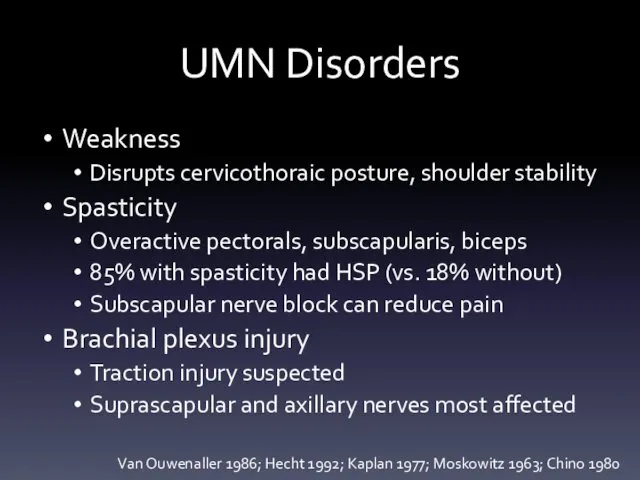
- 11. UMN Disorders Weakness Disrupts cervicothoraic posture, shoulder stability Spasticity Overactive pectorals, subscapularis, biceps 85% with spasticity
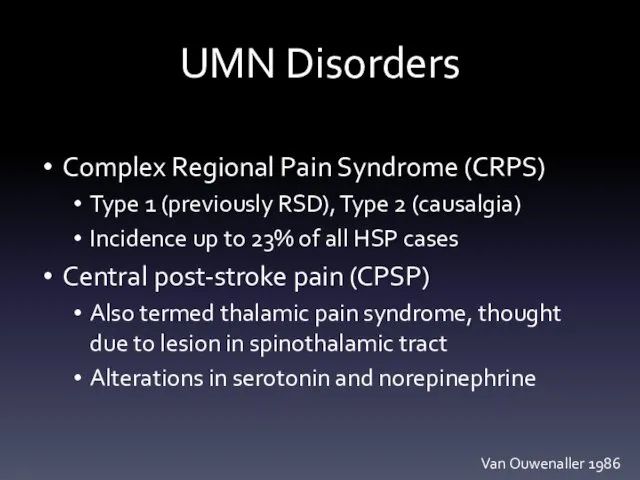
- 12. UMN Disorders Complex Regional Pain Syndrome (CRPS) Type 1 (previously RSD), Type 2 (causalgia) Incidence up
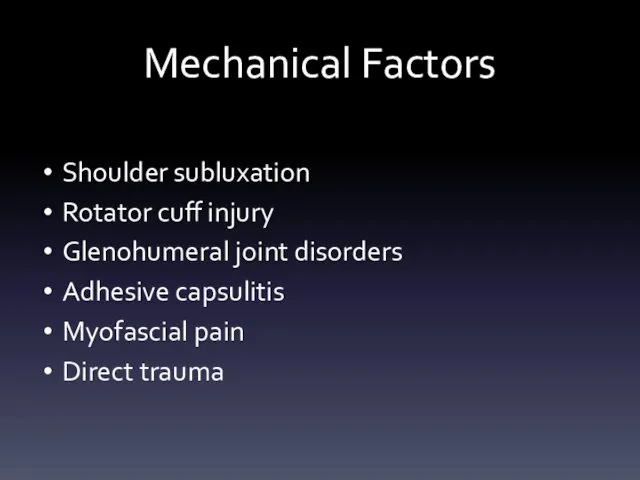
- 13. Mechanical Factors Shoulder subluxation Rotator cuff injury Glenohumeral joint disorders Adhesive capsulitis Myofascial pain Direct trauma
- 14. Diagnosis History, physical examination, special tests/maneuvers Imaging (XR, MRI, US) Electrodiagnosis Diagnostic injections (nerve, muscle, joint)
- 15. Diagnosis: Exam Observation ROM AROM, then PROM Palpation Assess for bulk, focal tenderness Sensation Dermatomes, peripheral
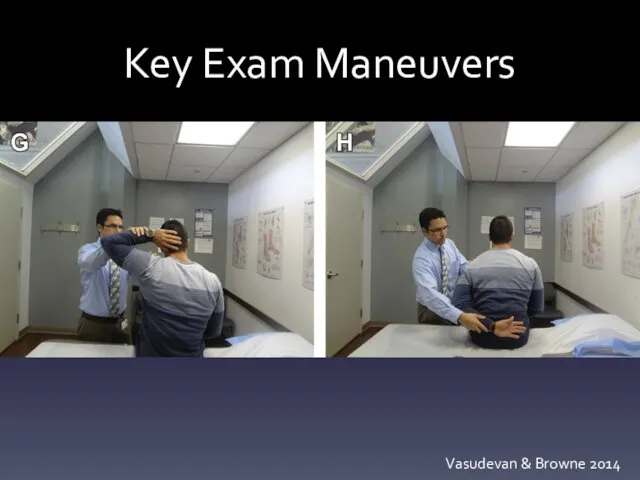
- 16. Diagnosis: Exam Special tests Neer, Hawkins, Jobe, O’Brien, HBB/HBN Instability: Apprehension, Sulcus Diagnostic Injections Nerve blocks
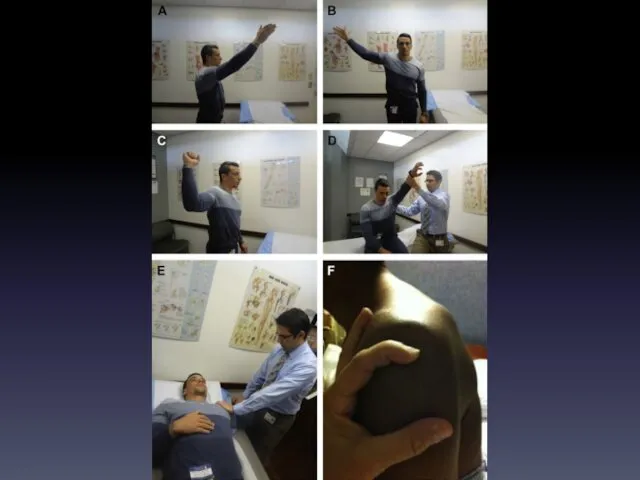
- 18. Key Exam Maneuvers Vasudevan & Browne 2014
- 19. Diagnosis: Imaging Radiography AP: assess for fracture, subluxation ER: calcific tendinopathy; IR: Hill-Sachs lesion Scapular Y:
- 20. Diagnosis: Imaging Relationship of imaging and HSP Lo et al study: HSP cohort: 50% adhesive capsulitis,
- 21. Management Prevention through positioning Flaccid stage: risk for injury Suggested: abduction, ER, flexion But no consensus,
- 22. Physical Therapy Mechanical Factors PROM exercises within pain-free range can reduce reports of shoulder pain by
- 23. Physical Therapy Neurogenic Factors TENS: high intensity > low intensity or placebo FES: to reduce shoulder
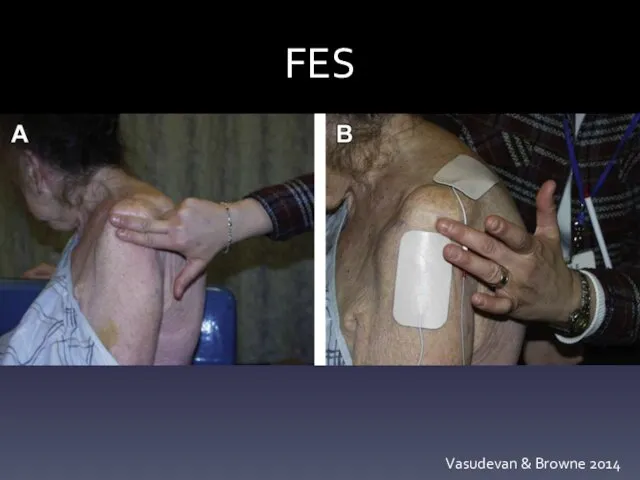
- 24. FES Vasudevan & Browne 2014
- 25. Physical Therapy Neurogenic Factors EMG biofeedback and relaxation: 150 min x 5 days biofeedback or 30
- 26. Interventional Neurogenic Factors Botulinum toxin (presynaptic Ach inhibitor) Several small studies show favorable results for both
- 27. Pharmacotherapy NSAIDs, topical lidocaine, antiepileptic agents, TCAs, SSRIs, antispasmodics The problem: not a single good trial
- 28. Complementary and alternative medicine Acupuncture Works via neurohormonal mechanism: β-endorphin dynorphin A/B, substance P, noradrenaline Benefit
- 29. Surgery Typically for adhesive capsulitis (release of capsular adhesions, manipulation under anesthesia) or rotator cuff tendinopathy
- 30. Suggested Protocol Step 1: Identify neurogenic factors Step 2: Identify mechanical factors Step 3: Prevention through
- 31. Suggested Protocol Strapping/Taping: perpendicular to inhibit, parallel to promote Slings: Flaccid: sitting, ambulating, transferring Spastic: avoid
- 32. Suggested Protocol Physical Therapy and Modalities Strive for maximal pain-free ROM Avoid overhead pulley exercises TENS:
- 33. Suggested Protocol Pharmacotherapy Neurogenic: Neuropathic pain: AEDs, TCAs, SSRIs Spasticity: antispasmodics Mechanical NSAIDs and acetaminophen Rare
- 34. Suggested Protocol Injection therapy Neurogenic: Botulinum Toxin: IM, possibly even IA Stellate Ganglion Block Mechanical Corticosteroid
- 35. Suggested Protocol Complementary and alternative medicine Acupuncture may be superior in combination with standard PT than
- 36. Suggested Protocol Surgery (after 6 mos failed conservative Tx) Neurogenic: release of contractures Mechanical: capsular release,
- 37. Summary HSP is a common complication of CVA which is known to be associated with poor
- 38. Objectives Identify the neurogenic and mechanical factors which contribute to HSP Prescribe appropriate treatments for the
- 39. References Contact me for a list john.vasudevan@uphs.upenn.edu Or see: Vasudevan J, Browne B. Hemiplegic shoulder pain:
- 41. Скачать презентацию
 Современная терапия неходжкинских лимфом - ритуксимаб
Современная терапия неходжкинских лимфом - ритуксимаб Пельвиоперитонит
Пельвиоперитонит Программа комплексной реабилитации лиц с нарушениями опорно-двигательного аппарата
Программа комплексной реабилитации лиц с нарушениями опорно-двигательного аппарата Неотложные состояния в торакальной хирургии
Неотложные состояния в торакальной хирургии Синдром гиперпролактинемии
Синдром гиперпролактинемии Травма. Виды травм
Травма. Виды травм Инфекции, вызываемые клостридиями
Инфекции, вызываемые клостридиями Аварийные ситуации-санитарки
Аварийные ситуации-санитарки Эффективность применения пассивной гимнастики в физической реабилитации для лиц после геморрагического инсульта
Эффективность применения пассивной гимнастики в физической реабилитации для лиц после геморрагического инсульта Биохимия тканей зуба и слюны
Биохимия тканей зуба и слюны Алкоголизм и его влияние на развитие здоровой личности
Алкоголизм и его влияние на развитие здоровой личности Дифференциация нарушений звукопроизношения при алалии и дизартрии: зависимость приемов коррекции от механизма нарушения
Дифференциация нарушений звукопроизношения при алалии и дизартрии: зависимость приемов коррекции от механизма нарушения Мышцы спины
Мышцы спины Опухоли головного мозга
Опухоли головного мозга Тістің қатты тіндерінің тісжегі емес ақауларының потоморфологиясы
Тістің қатты тіндерінің тісжегі емес ақауларының потоморфологиясы Кто такие левши?. (8 класс)
Кто такие левши?. (8 класс) Situația epidemiologică privind infecția covid-19
Situația epidemiologică privind infecția covid-19 Психофармакогенетика. Понятие генетического полиморфизма
Психофармакогенетика. Понятие генетического полиморфизма Эндокринология. Феохромоцитома
Эндокринология. Феохромоцитома ҚШҰ-синдромы. Шок жалпыпатологилық сырқат ретінде. Үрдістердің патоморфологиясы
ҚШҰ-синдромы. Шок жалпыпатологилық сырқат ретінде. Үрдістердің патоморфологиясы Болезнь Осгуда-Шляттера
Болезнь Осгуда-Шляттера Diagnosis and management of VUR after first UTI
Diagnosis and management of VUR after first UTI Хронический гастрит. Язвенная болезнь
Хронический гастрит. Язвенная болезнь Понятие здоровья. Современные методы и подходы к изучению здоровья
Понятие здоровья. Современные методы и подходы к изучению здоровья Третий период родов и послеродовый период
Третий период родов и послеродовый период Диагностический поиск при вирусных гепатитах. Клиническо-эпидемиологические и лабораторные критерии диагностики гепатитов
Диагностический поиск при вирусных гепатитах. Клиническо-эпидемиологические и лабораторные критерии диагностики гепатитов Острые заболевания верхних дыхательных путей в практике участкового терапевта
Острые заболевания верхних дыхательных путей в практике участкового терапевта Шигеллёз
Шигеллёз