Содержание
- 2. Henoch-Schönlein Purpura (HSP) is a common vasculitis of small vessels with cutaneous and systemic complications. It
- 3. EPIDEMIOLOGY The etiology is unknown more frequent in children than adults, with most cases occurring between
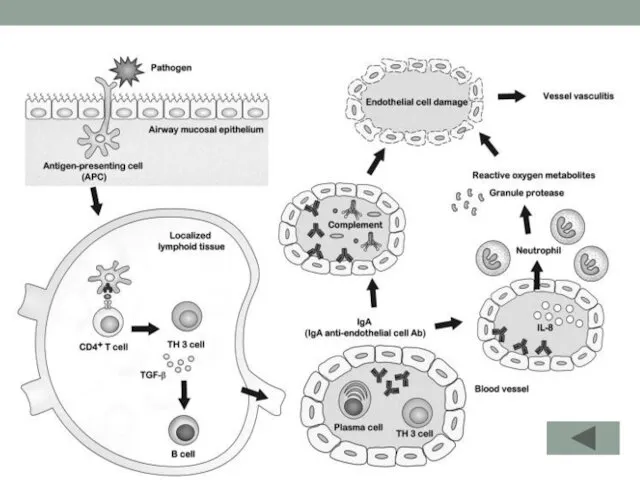
- 4. PATHOGENESIS in specific populations, patients with HSP have a significantly higher frequency of HLA-DRB1*01 and decreased
- 5. CTLA-4 +49 A/G genotype and HLA-DRB1 polymorphisms in Turkish patients with Henoch-Schönlein purpura. presence of Cytotoxic
- 7. The immunobiology of Henoch-Schönlein purpura. group A beta-hemolytic streptococcus (GAS) has widely studied and found in
- 8. CLINICAL MANIFESTATIONS The disease onset may be acute, or insidious, with sequential occurrence of symptoms over
- 9. CLINICAL MANIFESTATIONS Rash (95-100%), especially involving the legs, may not be present on initial presentation Subcutaneous
- 10. Rash beginning as pinkish maculopapules that initially blanch on pressure and progress to petechiae or purpura,
- 11. Rash
- 12. Arthritis present in more than ⅔ of children with HSP, is usually localized to the knees
- 13. Gastrointestinal tract intermittent abdominal pain that is often colicky in nature. There may be peritoneal exudate,
- 14. Renal involvement occurs in 25-50% of children may manifest with: hematuria, proteinuria, or both; nephritis or
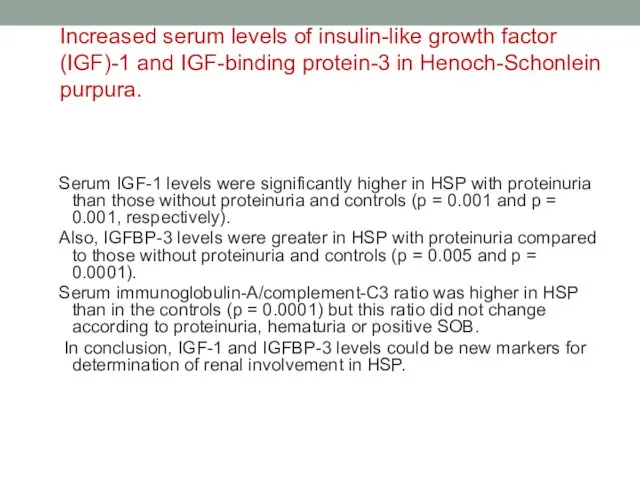
- 15. Increased serum levels of insulin-like growth factor (IGF)-1 and IGF-binding protein-3 in Henoch-Schonlein purpura. Serum IGF-1
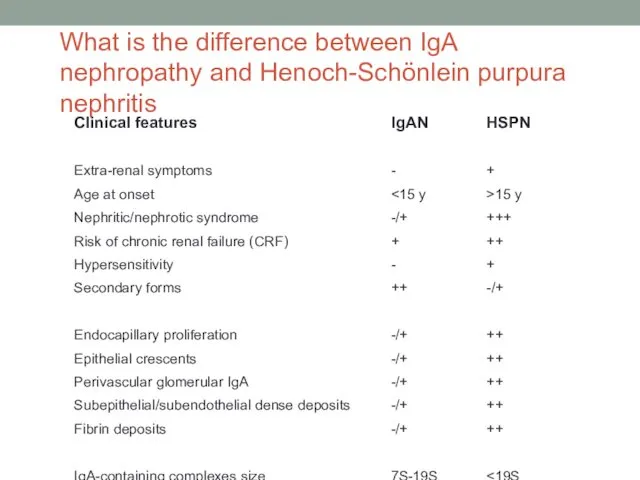
- 16. What is the difference between IgA nephropathy and Henoch-Schönlein purpura nephritis
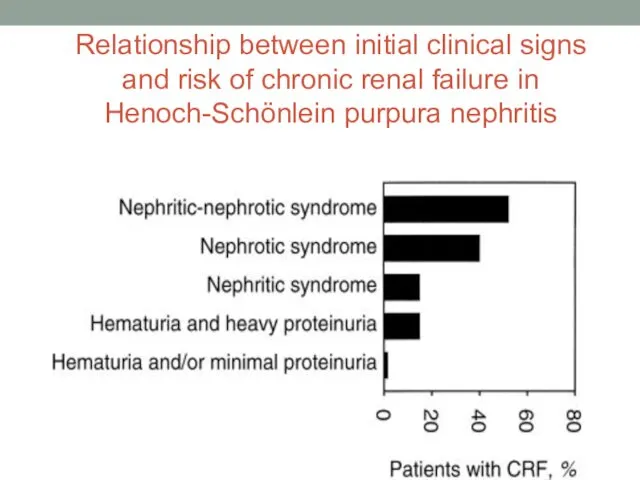
- 17. Relationship between initial clinical signs and risk of chronic renal failure in Henoch-Schönlein purpura nephritis
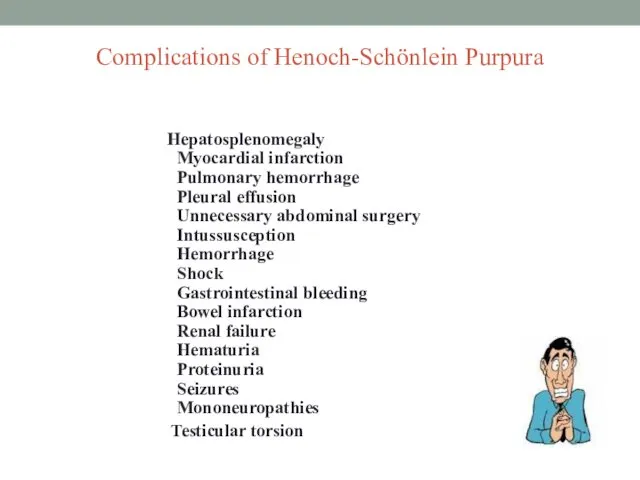
- 18. Complications of Henoch-Schönlein Purpura Hepatosplenomegaly Myocardial infarction Pulmonary hemorrhage Pleural effusion Unnecessary abdominal surgery Intussusception Hemorrhage
- 19. DIAGNOSIS Diagnostic uncertainty arises when the symptom complex of edema, rash, arthritis with abdominal complaints, and
- 20. DIAGNOSIS Affected children often have a moderate thrombocytosis and leukocytosis. The erythrocyte sedimentation rate (ESR) may
- 21. Definitive diagnosis confirmed by biopsy cutaneous site showing leukocytoclastic angiitis. Renal biopsy may show mesangial deposition
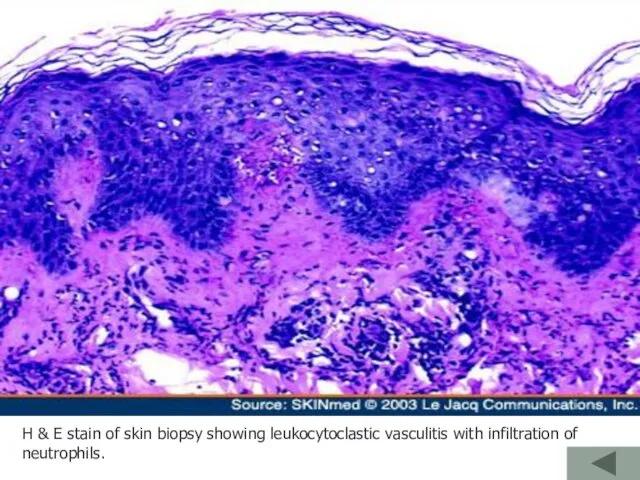
- 22. H & E stain of skin biopsy showing leukocytoclastic vasculitis with infiltration of neutrophils.
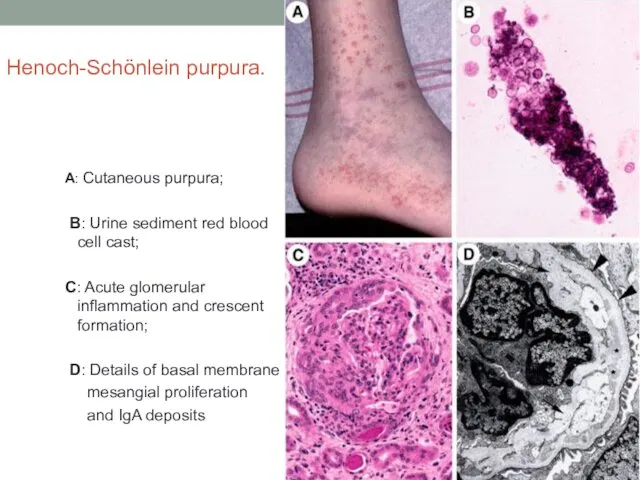
- 23. Henoch-Schönlein purpura. A: Cutaneous purpura; B: Urine sediment red blood cell cast; C: Acute glomerular inflammation
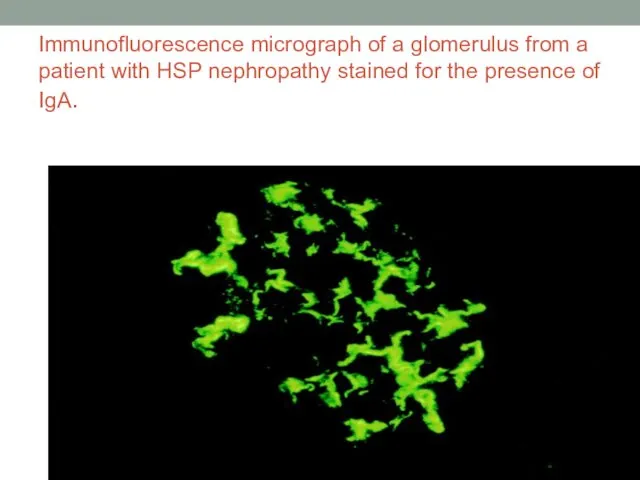
- 24. Immunofluorescence micrograph of a glomerulus from a patient with HSP nephropathy stained for the presence of
- 25. Differential Diagnosis of Henoch-Schönlein Purpura Acute abdomen Meningococcal meningitis or septicemia Rheumatoid arthritis Rheumatic fever Idiopathic
- 26. Acute hemorrhagic edema (AHE) is an acute cutaneous benign leukocytoclastic vasculitis seen in children ≤2 yr
- 27. Acute hemorrhagic edema (AHE)
- 28. TREATMENT Symptomatic treatment adequate hydration, bland diet, pain control with acetaminophen is provided for self-limited complaints
- 29. TREATMENT Therapy with oral or intravenous corticosteroids (1-2 mg/kg/day) is often associated with dramatic improvement of
- 30. TREATMENT is the same as for other forms of acute glomerulonephritis If anti-cardiolipin or antiphospholipid antibodies
- 31. Prognosis More than 80% of patients have a single isolated episode lasting a few weeks. Approximately
- 33. Скачать презентацию


 Отклонение в интеллектуальном развитии у детей
Отклонение в интеллектуальном развитии у детей Кожный шов
Кожный шов Спілкування – це процес встановлення і розвитку контакту між людьми. Лекція №4
Спілкування – це процес встановлення і розвитку контакту між людьми. Лекція №4 Физиология системы выделения. Функции почек. Механизмы мочеобразования
Физиология системы выделения. Функции почек. Механизмы мочеобразования Возбудитель сибирской язвы
Возбудитель сибирской язвы Сахарный диабет
Сахарный диабет Гинекологиялық операциялардан кейінгі науқастардың тамақтануы
Гинекологиялық операциялардан кейінгі науқастардың тамақтануы Задачи, организационная структура и основы деятельности Всероссийской службы медицины катастроф
Задачи, организационная структура и основы деятельности Всероссийской службы медицины катастроф Практикум по методам психологического исследования. Лабораторное занятие № 1
Практикум по методам психологического исследования. Лабораторное занятие № 1 Наркотики
Наркотики Гигиена кожи
Гигиена кожи Охрана зрения слабовидящего дошкольника
Охрана зрения слабовидящего дошкольника Врачевание на средневековом востоке
Врачевание на средневековом востоке Медична гельмінтологія. Плоскі та круглі черви паразити людини
Медична гельмінтологія. Плоскі та круглі черви паразити людини Франшиза: медицинский центр профилактики
Франшиза: медицинский центр профилактики Множественная лекарственная устойчивость МБТ
Множественная лекарственная устойчивость МБТ Уход за больными с повреждениями позвоночника, спинного мозга, таза
Уход за больными с повреждениями позвоночника, спинного мозга, таза Инсульт. Статистика инсульта
Инсульт. Статистика инсульта Человек и его здоровье. Кровь. Кровообращение
Человек и его здоровье. Кровь. Кровообращение Стандартизация в медицине и здравоохранении
Стандартизация в медицине и здравоохранении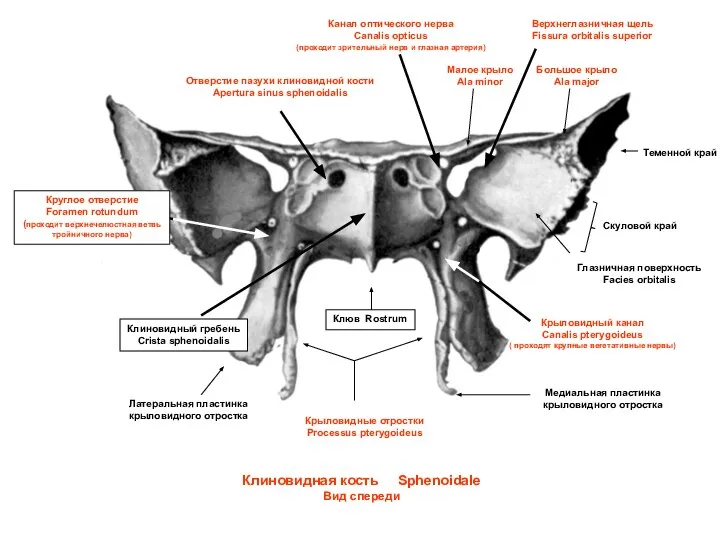 Клиновидная кость. Вид спереди
Клиновидная кость. Вид спереди Инсульттер кезіндегі алғашқы көмек алгоритмі
Инсульттер кезіндегі алғашқы көмек алгоритмі Медико-социальные аспекты демографии
Медико-социальные аспекты демографии Аттестационная работа. Влияние на организм младшего школьника компьютерных и подвижных игр
Аттестационная работа. Влияние на организм младшего школьника компьютерных и подвижных игр Гостра ревматична лихоманка у дітей
Гостра ревматична лихоманка у дітей Потапова А.С
Потапова А.С Некротическая флегмона новорожденных
Некротическая флегмона новорожденных Основы доказательной медицины
Основы доказательной медицины