Содержание
- 2. About these slides These slides give a comprehensive overview of the EASL clinical practice guidelines on
- 3. About these slides Definitions of all abbreviations shown in these slides are provided within the slide
- 4. Guideline panel EASL CPG PBC. J Hepatol 2017;67:145–72 Chair Gideon M Hirschfield Panel members Ulrich Beuers,
- 5. Outline EASL CPG PBC. J Hepatol 2017;67:145–72
- 6. Methods Grading evidence and recommendations
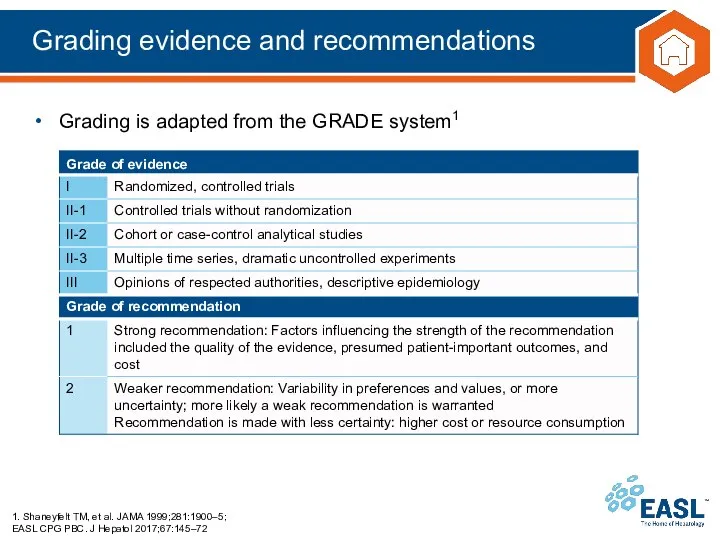
- 7. Grading evidence and recommendations 1. Shaneyfelt TM, et al. JAMA 1999;281:1900–5; EASL CPG PBC. J Hepatol
- 8. Background Epidemiology of PBC PBC pathogenesis
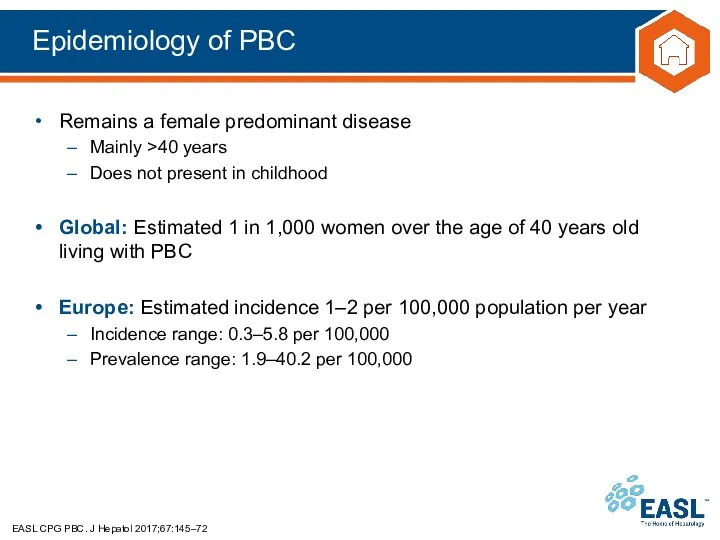
- 9. Epidemiology of PBC EASL CPG PBC. J Hepatol 2017;67:145–72 Remains a female predominant disease Mainly >40
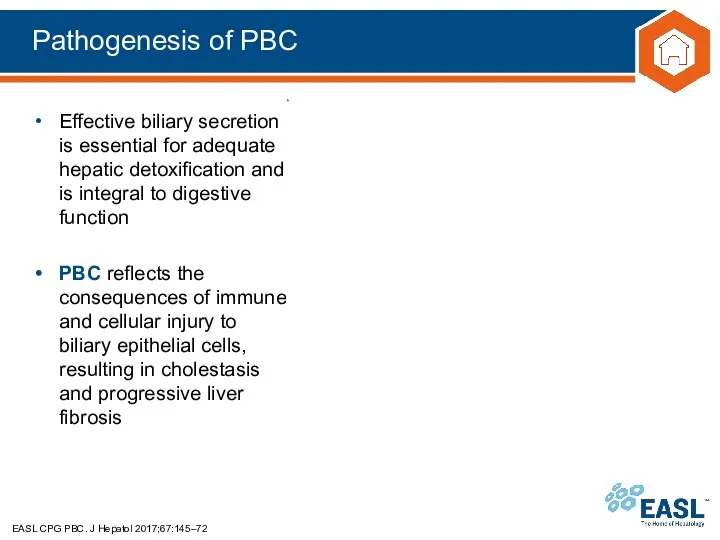
- 10. Pathogenesis of PBC EASL CPG PBC. J Hepatol 2017;67:145–72 Effective biliary secretion is essential for adequate
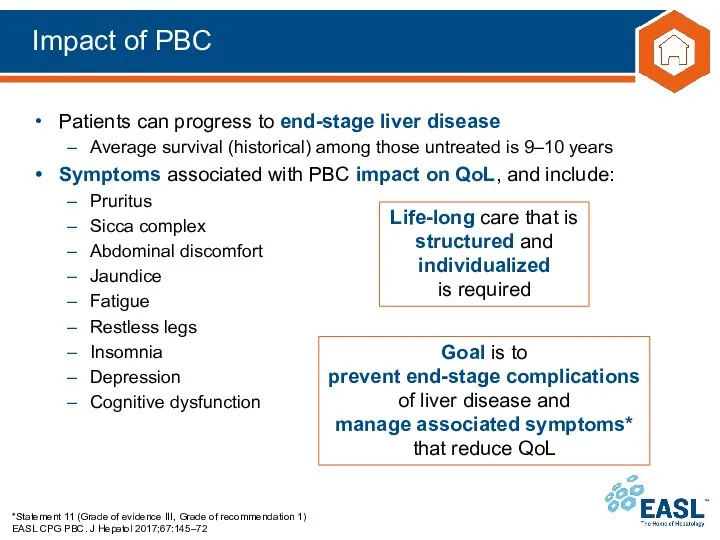
- 11. Impact of PBC *Statement 11 (Grade of evidence III, Grade of recommendation 1) EASL CPG PBC.
- 12. Guidelines Key recommendations
- 13. Topics EASL CPG PBC. J Hepatol 2017;67:145–72 Diagnostic approach to cholestasis Initial diagnosis of PBC Stratification
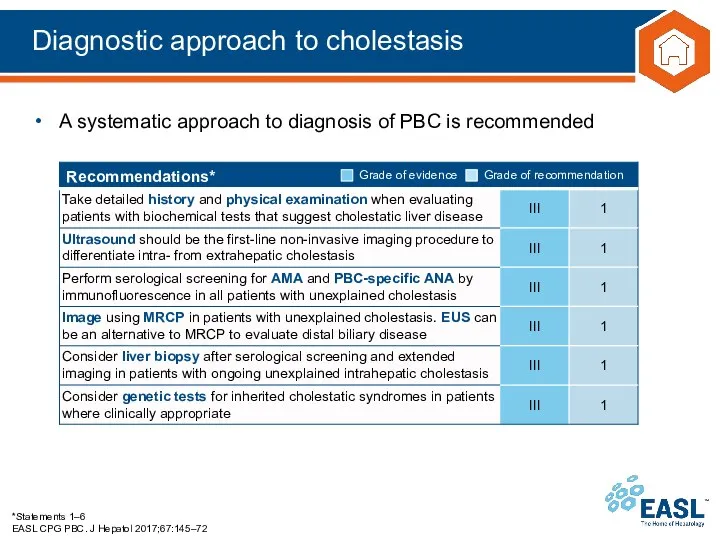
- 14. Diagnostic approach to cholestasis *Statements 1–6 EASL CPG PBC. J Hepatol 2017;67:145–72 A systematic approach to
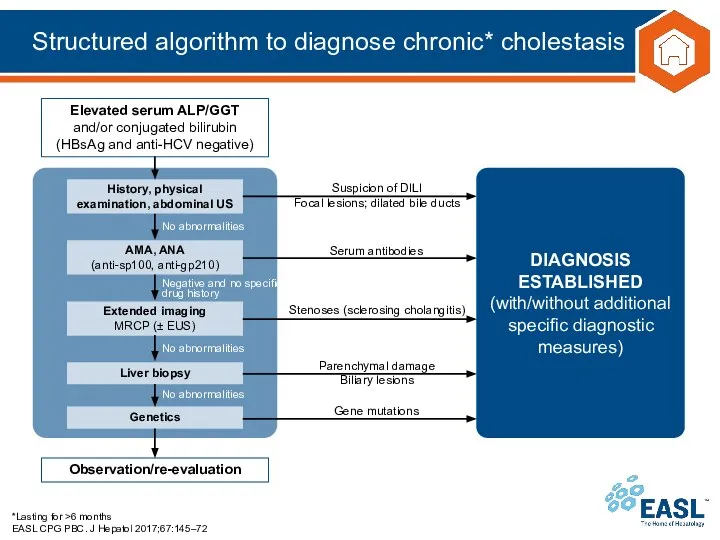
- 15. Structured algorithm to diagnose chronic* cholestasis *Lasting for >6 months EASL CPG PBC. J Hepatol 2017;67:145–72
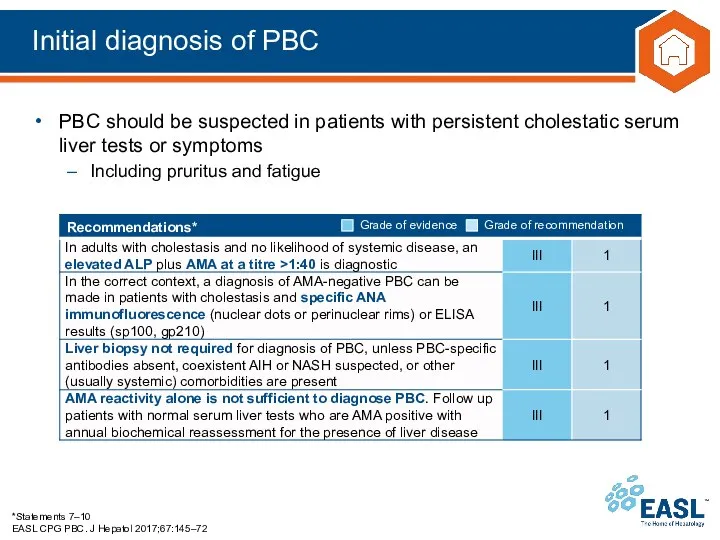
- 16. Initial diagnosis of PBC *Statements 7–10 EASL CPG PBC. J Hepatol 2017;67:145–72 PBC should be suspected
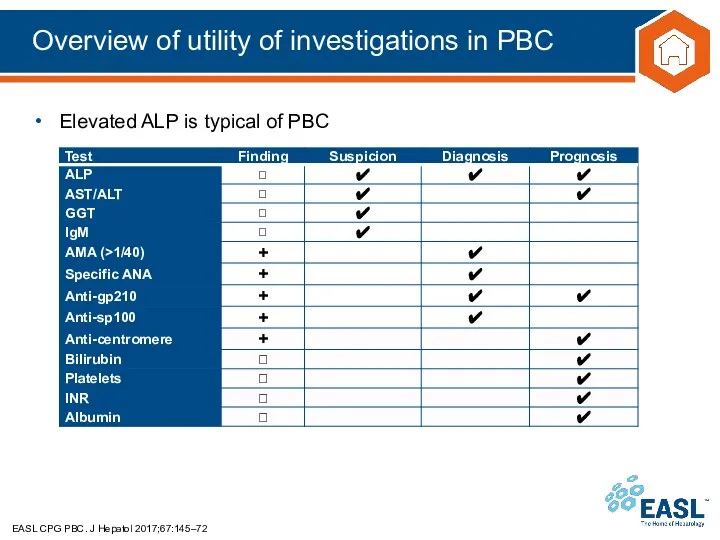
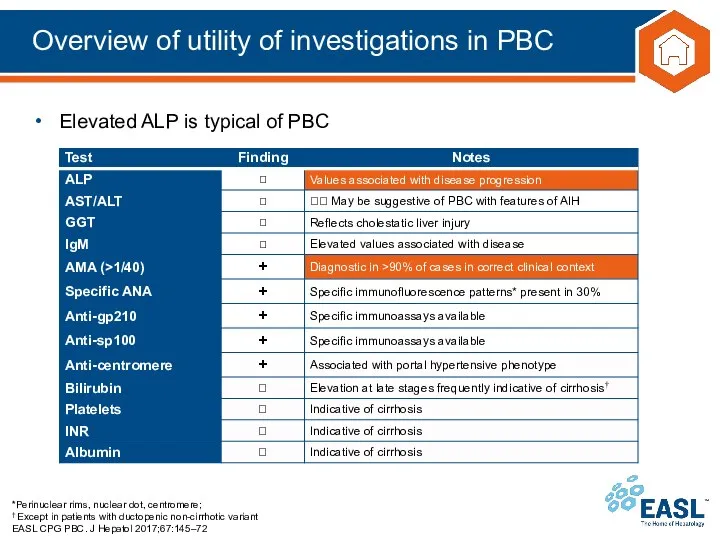
- 17. Overview of utility of investigations in PBC EASL CPG PBC. J Hepatol 2017;67:145–72 Elevated ALP is
- 18. Overview of utility of investigations in PBC *Perinuclear rims, nuclear dot, centromere; † Except in patients
- 19. Histopathological features of PBC EASL CPG PBC. J Hepatol 2017;67:145–72 Liver biopsy is not generally required
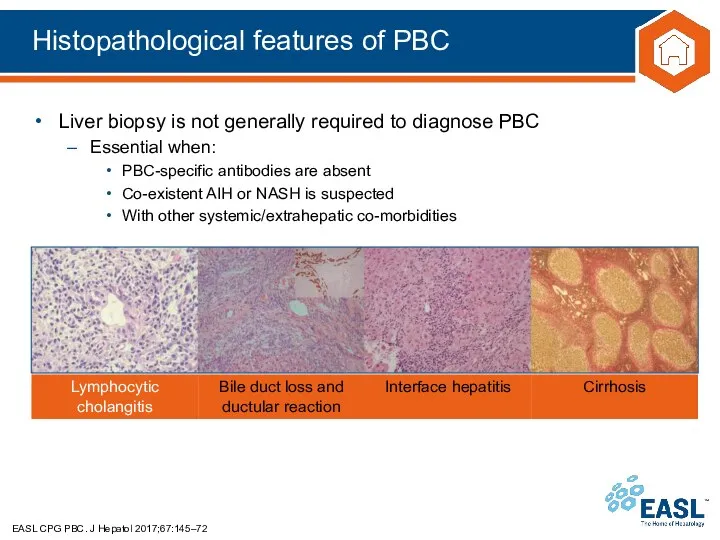
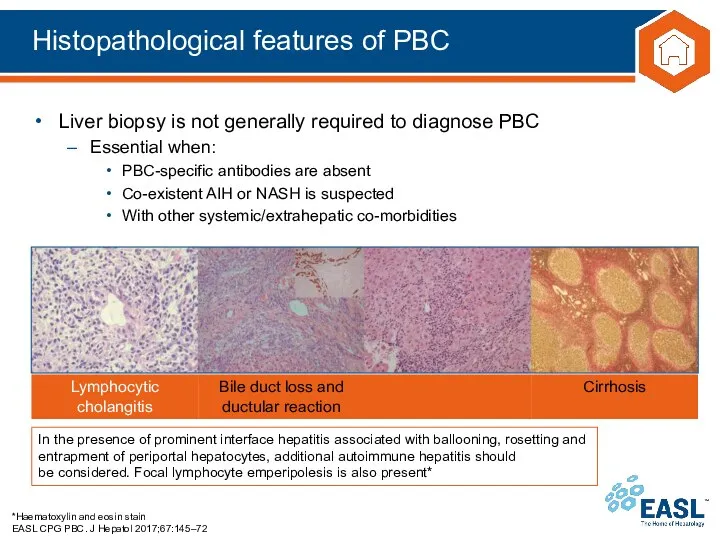
- 20. Histopathological features of PBC *Haematoxylin and eosin stain EASL CPG PBC. J Hepatol 2017;67:145–72 Liver biopsy
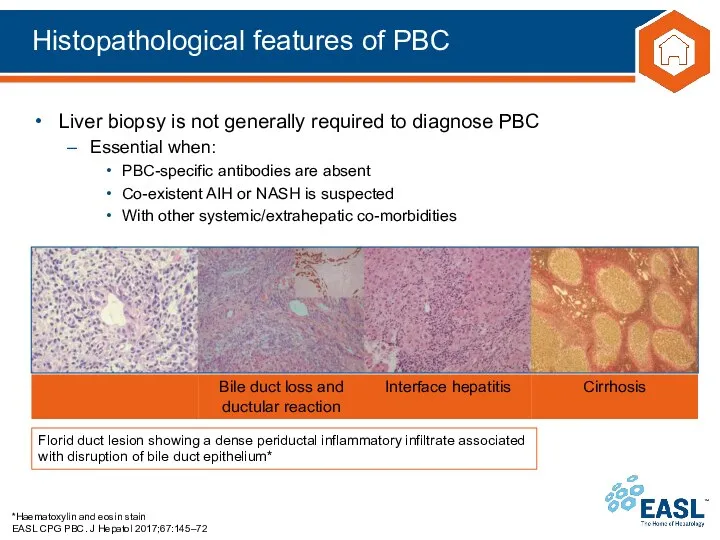
- 21. Histopathological features of PBC *Haematoxylin and eosin stain; †Immunostaining for keratin 7 with immunoperoxidase EASL CPG
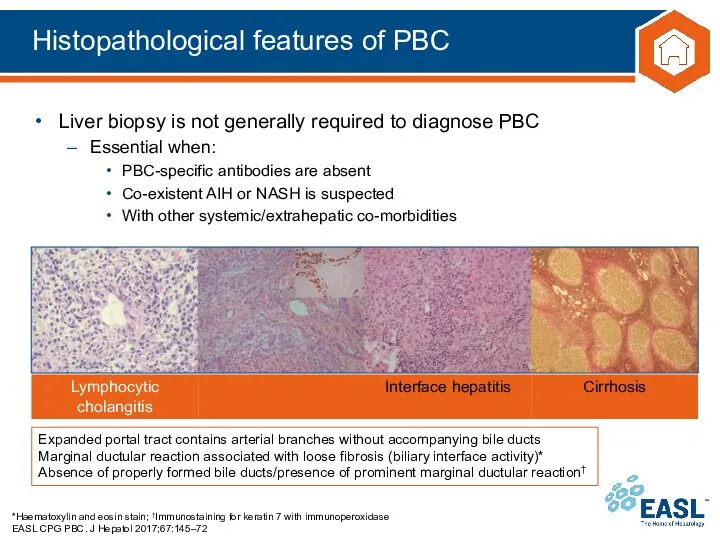
- 22. Histopathological features of PBC *Haematoxylin and eosin stain EASL CPG PBC. J Hepatol 2017;67:145–72 Liver biopsy
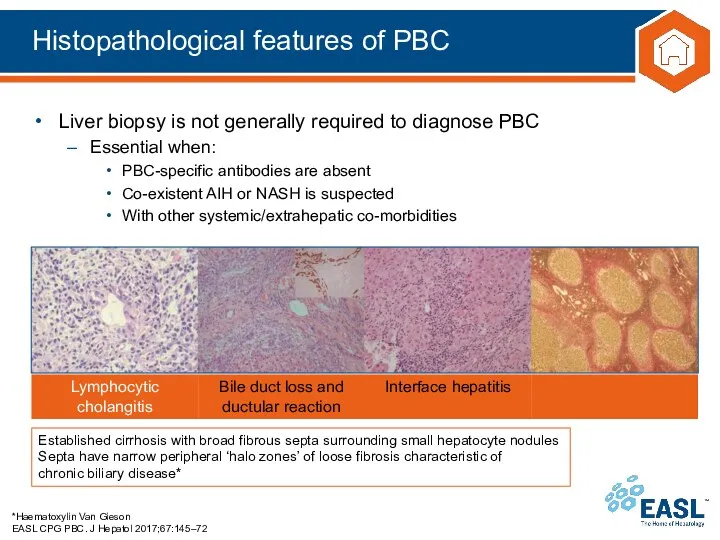
- 23. Histopathological features of PBC *Haematoxylin Van Gieson EASL CPG PBC. J Hepatol 2017;67:145–72 Liver biopsy is
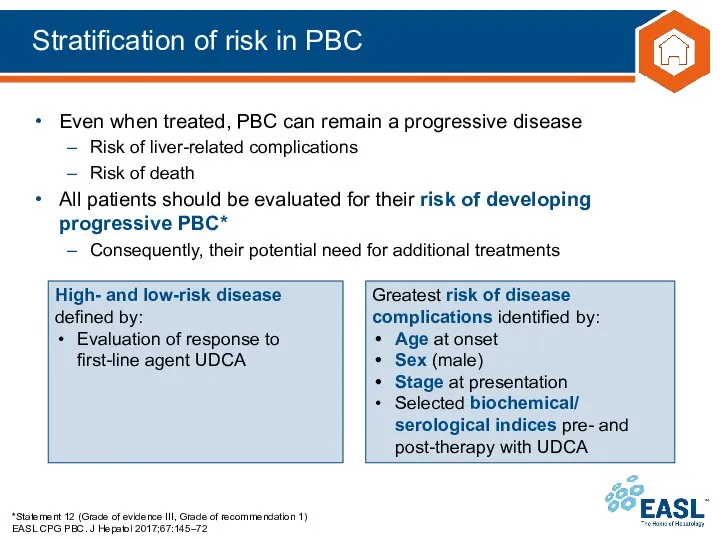
- 24. Stratification of risk in PBC *Statement 12 (Grade of evidence III, Grade of recommendation 1) EASL
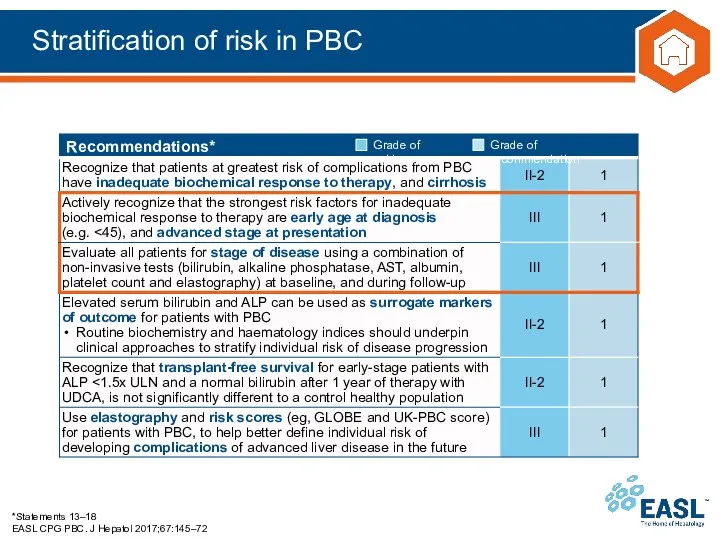
- 25. Stratification of risk in PBC *Statements 13–18 EASL CPG PBC. J Hepatol 2017;67:145–72
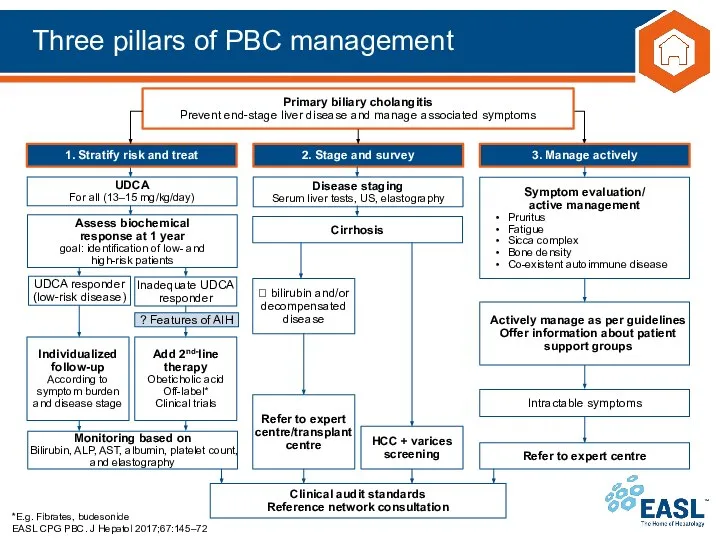
- 26. Three pillars of PBC management *E.g. Fibrates, budesonide EASL CPG PBC. J Hepatol 2017;67:145–72
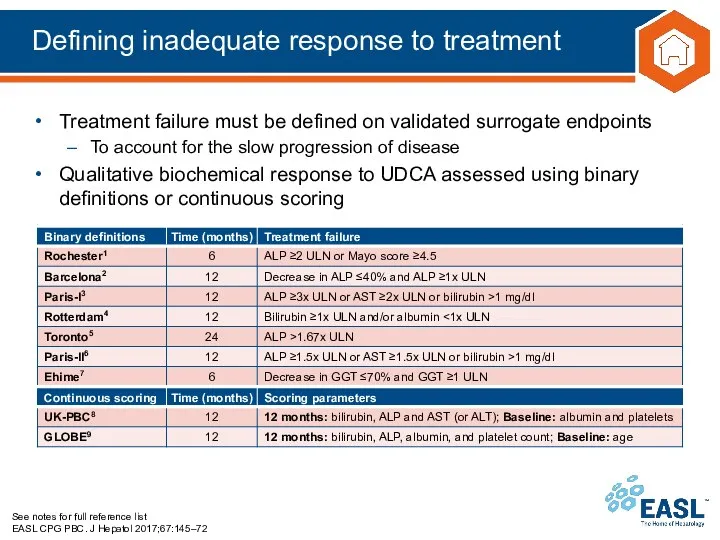
- 27. Defining inadequate response to treatment See notes for full reference list EASL CPG PBC. J Hepatol
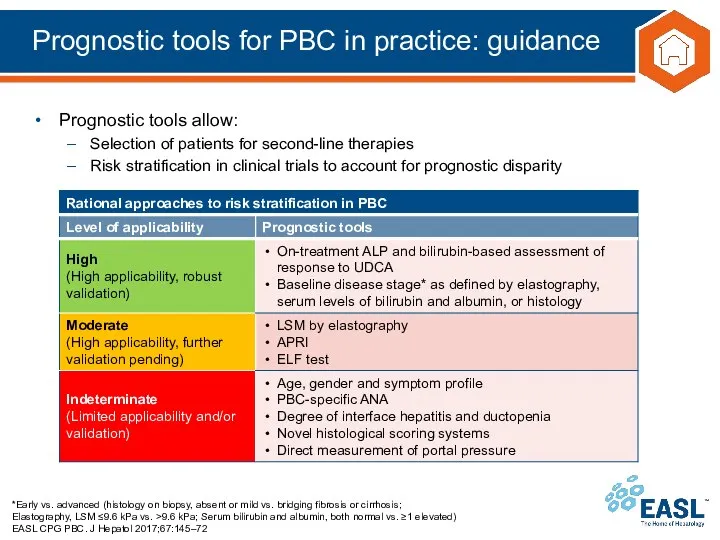
- 28. Prognostic tools for PBC in practice: guidance *Early vs. advanced (histology on biopsy, absent or mild
- 29. Treatment: therapies to slow disease progression *Statements 19–21 EASL CPG PBC. J Hepatol 2017;67:145–72 Ursodeoxycholic acid
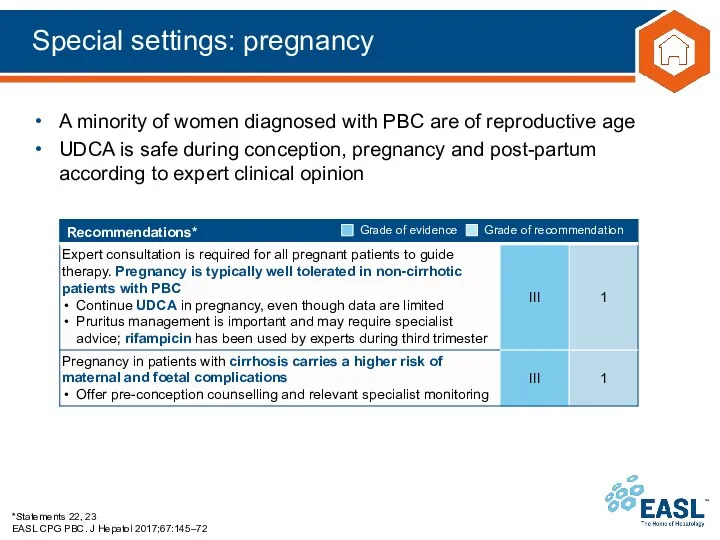
- 30. Special settings: pregnancy *Statements 22, 23 EASL CPG PBC. J Hepatol 2017;67:145–72 A minority of women
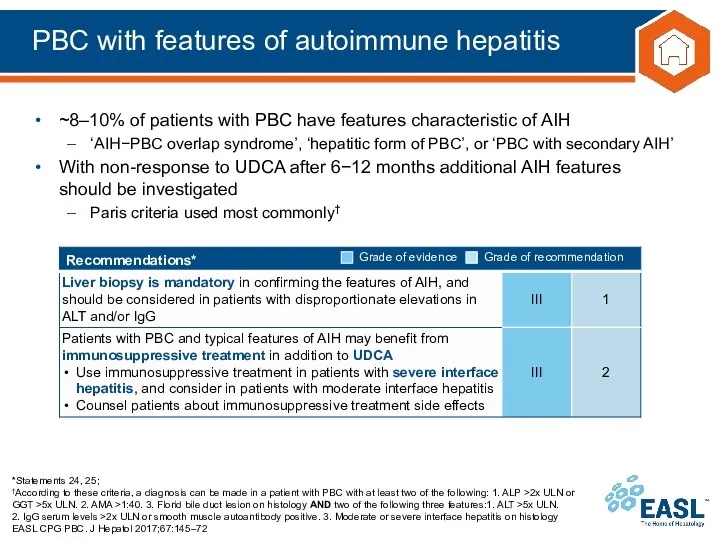
- 31. PBC with features of autoimmune hepatitis *Statements 24, 25; †According to these criteria, a diagnosis can
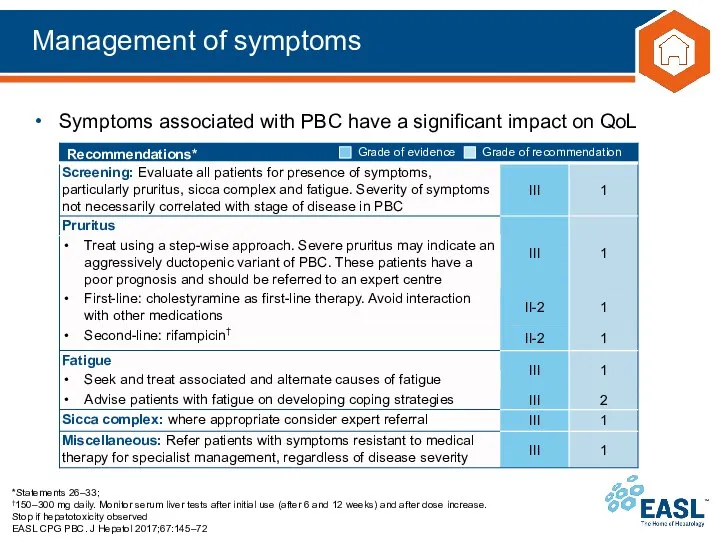
- 32. Management of symptoms *Statements 26–33; †150–300 mg daily. Monitor serum liver tests after initial use (after
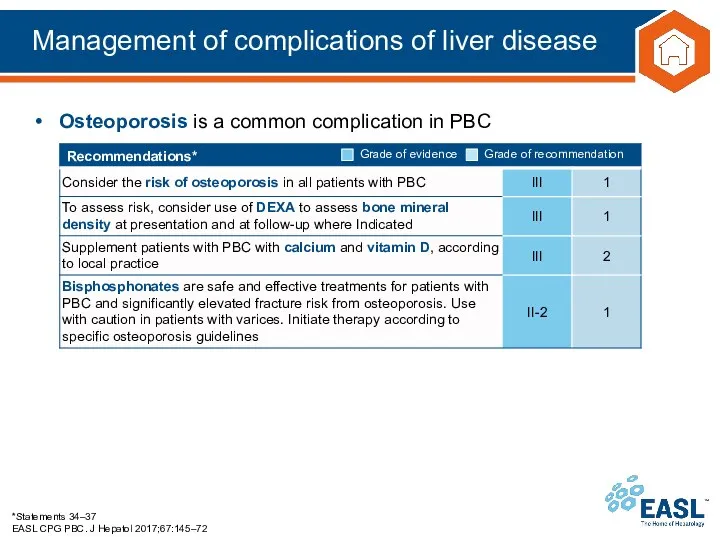
- 33. Management of complications of liver disease *Statements 34–37 EASL CPG PBC. J Hepatol 2017;67:145–72 Osteoporosis is
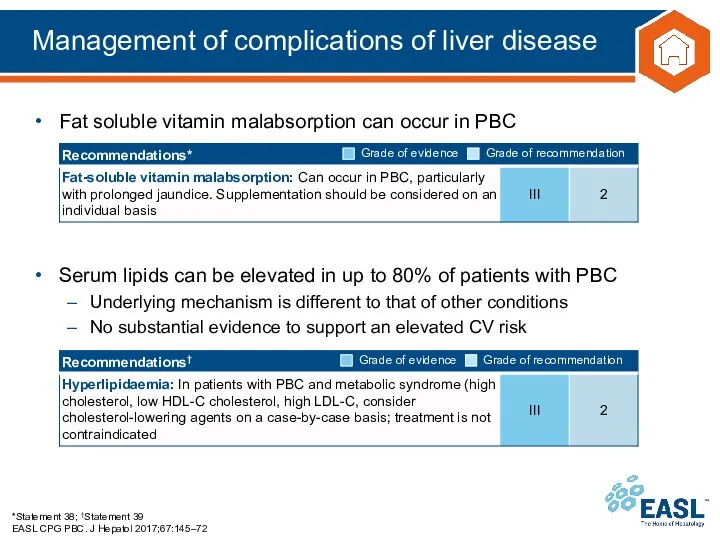
- 34. Management of complications of liver disease *Statement 38; †Statement 39 EASL CPG PBC. J Hepatol 2017;67:145–72
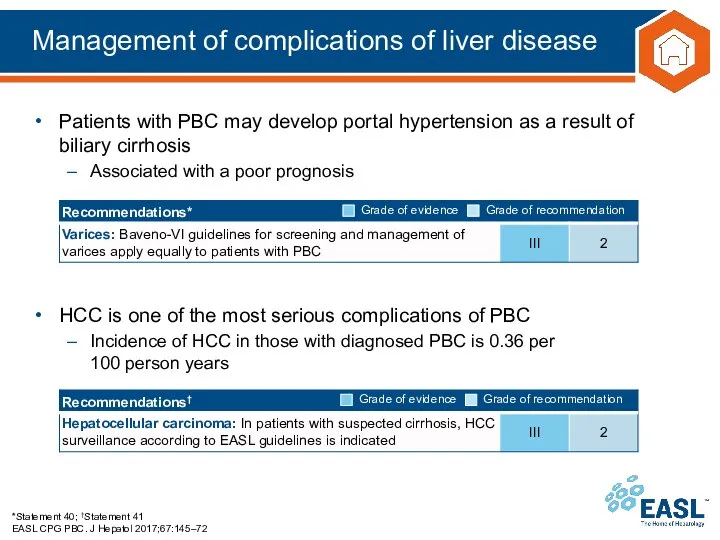
- 35. Management of complications of liver disease *Statement 40; †Statement 41 EASL CPG PBC. J Hepatol 2017;67:145–72
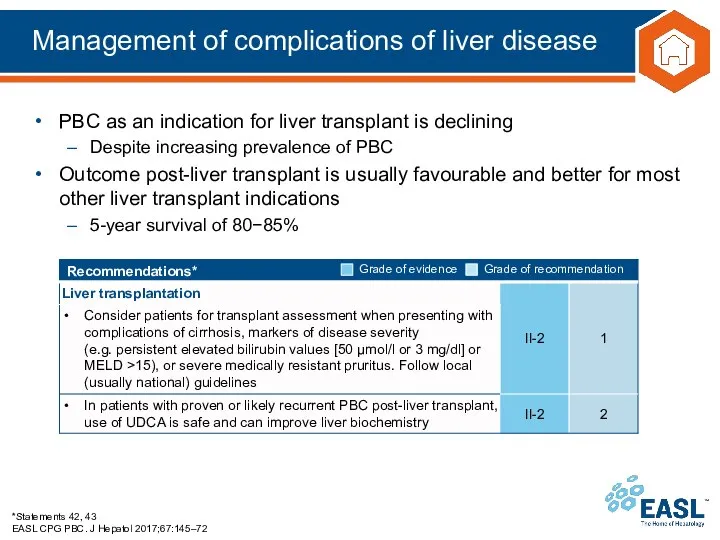
- 36. Management of complications of liver disease *Statements 42, 43 EASL CPG PBC. J Hepatol 2017;67:145–72 PBC
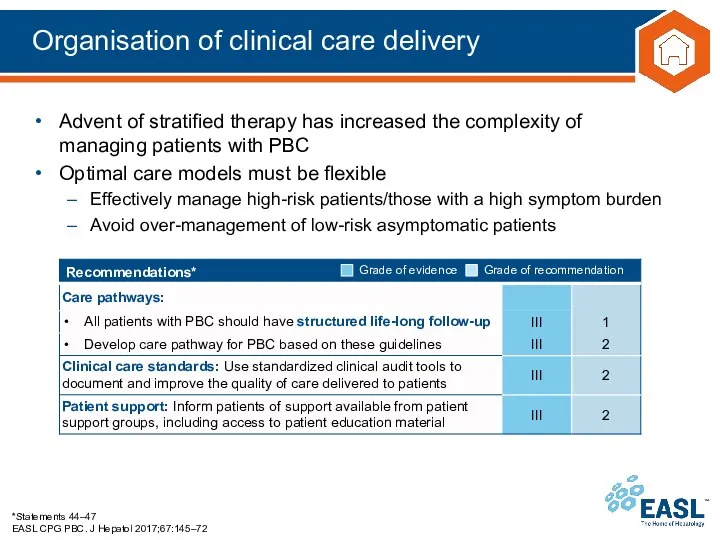
- 37. Organisation of clinical care delivery *Statements 44–47 EASL CPG PBC. J Hepatol 2017;67:145–72 Advent of stratified
- 39. Скачать презентацию

 Профессия врач – офтальмолог
Профессия врач – офтальмолог Базовые навыки в хирургии
Базовые навыки в хирургии Методы диагностики плода
Методы диагностики плода Спид и его профилактика (урок 4 - 11)
Спид и его профилактика (урок 4 - 11) Первая помощь при укусах животных
Первая помощь при укусах животных Диетотерапия при ОКИ
Диетотерапия при ОКИ Metody Rozpoznawania Płodności MRP. Dla ludzi chcących żyć zgodnie ze swoją płodnością
Metody Rozpoznawania Płodności MRP. Dla ludzi chcących żyć zgodnie ze swoją płodnością Кадровая политика, подготовка медицинских кадров и взаимодействие с медицинскими ВУЗами в Нижегородской области
Кадровая политика, подготовка медицинских кадров и взаимодействие с медицинскими ВУЗами в Нижегородской области Тяжелая внебольничная пневмония
Тяжелая внебольничная пневмония Заттың рентгендік сәулемен әрекеттесуі
Заттың рентгендік сәулемен әрекеттесуі Методы диагностики дисфункции плаценты
Методы диагностики дисфункции плаценты Туберкулез легких
Туберкулез легких Өлкелік инфекциялық патологияны зерттеудегі отандық ғалымдардың рөлі
Өлкелік инфекциялық патологияны зерттеудегі отандық ғалымдардың рөлі Антиангинальные и антиишемические средства. Коронарная болезнь сердца
Антиангинальные и антиишемические средства. Коронарная болезнь сердца Применение Nd:YAG лазера для фототермической реконструкции стенок влагалища
Применение Nd:YAG лазера для фототермической реконструкции стенок влагалища Жұқпалы аурулардың тасылып әкелуінен және таралуынан ел аумағын санитарлық қорғау
Жұқпалы аурулардың тасылып әкелуінен және таралуынан ел аумағын санитарлық қорғау Жүктілік кезіндегі аналық без кистасы
Жүктілік кезіндегі аналық без кистасы Современные клинико-фармакологические подходы к лечению аллергических заболеваний
Современные клинико-фармакологические подходы к лечению аллергических заболеваний Приспособительные и компенсаторные процессы
Приспособительные и компенсаторные процессы Азбука правильного питания
Азбука правильного питания колибактериоз
колибактериоз Наркотические анальгетики
Наркотические анальгетики Притча о гвоздях
Притча о гвоздях Вегетарианство: за или против
Вегетарианство: за или против Өкпе хирургиясында науқасты арнайы және жалпы отаға дайындау
Өкпе хирургиясында науқасты арнайы және жалпы отаға дайындау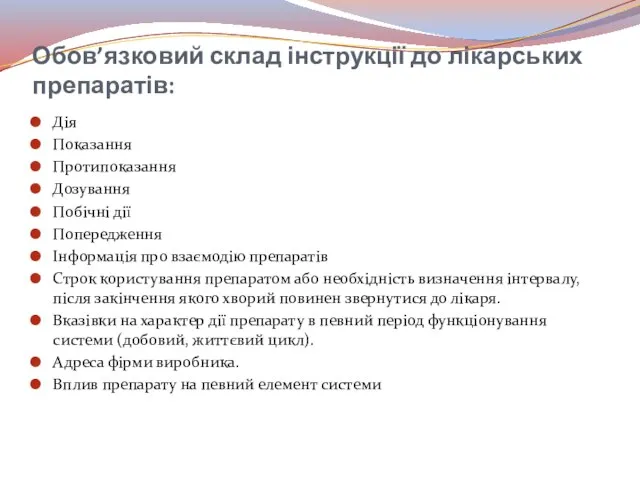 Обов’язковий склад інструкції до лікарських препаратів
Обов’язковий склад інструкції до лікарських препаратів Проблема ВИЧ/СПИД в Забайкальском крае
Проблема ВИЧ/СПИД в Забайкальском крае История вопроса возникновения COVID-19
История вопроса возникновения COVID-19