Содержание
- 2. Japanese encephalitis is a mosquito-borne viral infection of horses, pigs and humans. It is also referred
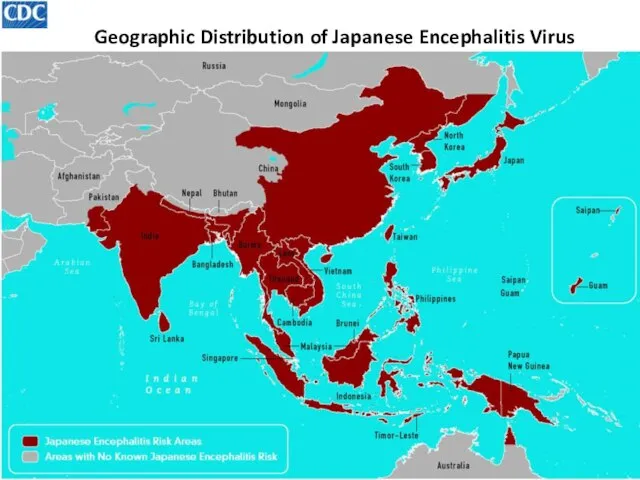
- 3. Geographic Distribution of Japanese Encephalitis Virus
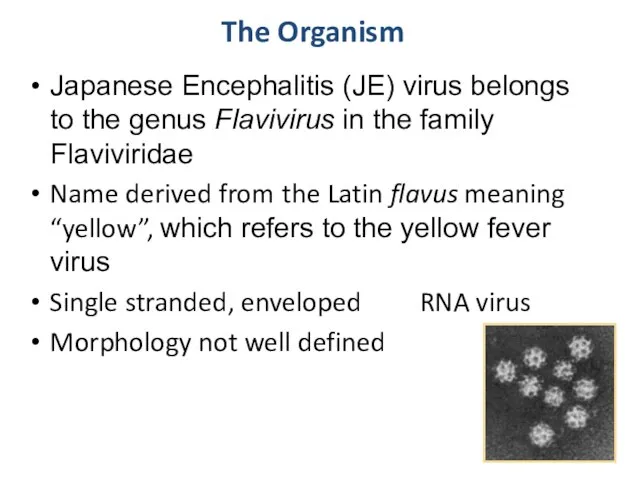
- 4. The Organism Japanese Encephalitis (JE) virus belongs to the genus Flavivirus in the family Flaviviridae Name
- 5. History 1870s: Japan “Summer encephalitis” epidemics 1924: Great epidemic in Japan 6,125 human cases; 3,797 deaths
- 6. History 1940 to 1978 Disease spread with epidemics in China, Korea, and India 1983: Immunization in
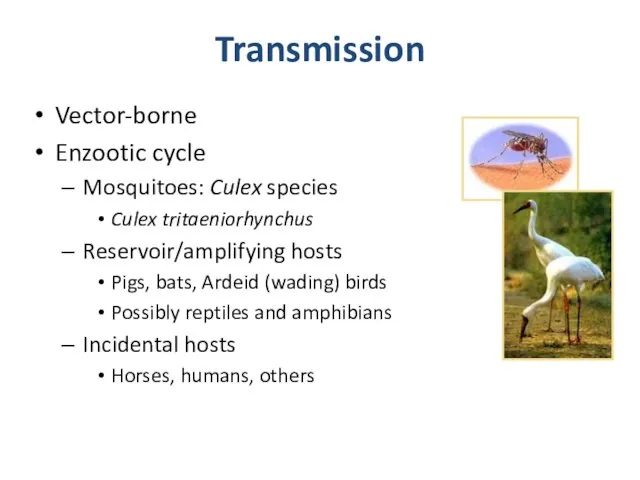
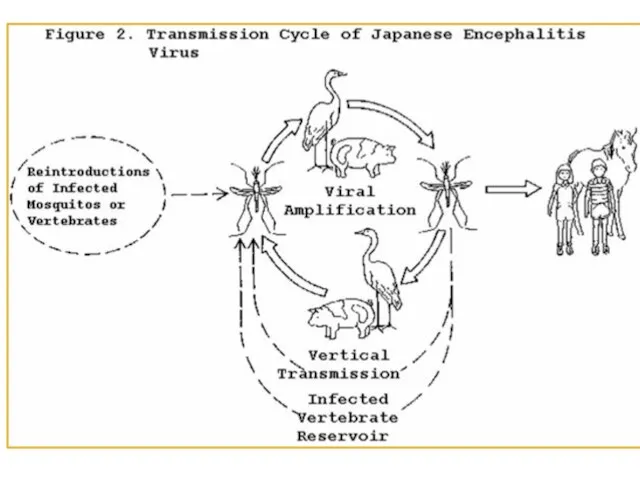
- 7. Transmission Vector-borne Enzootic cycle Mosquitoes: Culex species Culex tritaeniorhynchus Reservoir/amplifying hosts Pigs, bats, Ardeid (wading) birds
- 9. Transmission is usually seasonal In temperate zones of China, Japan, Korea and northern areas of Southeast
- 10. Clinical Signs Every year approximately 35,000 to 50,000 symptomatic cases occur worldwide Incubation period: 6 to
- 11. Clinical Signs: Severe Acute encephalitis Headache, high fever, stiff neck, stupor May progress to paralysis, seizures,
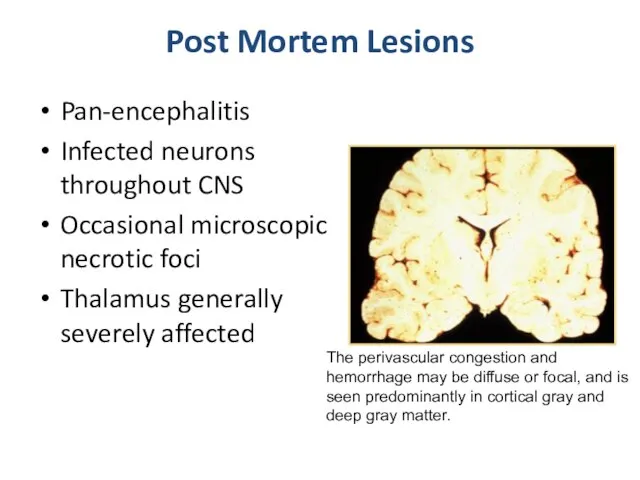
- 16. Post Mortem Lesions Pan-encephalitis Infected neurons throughout CNS Occasional microscopic necrotic foci Thalamus generally severely affected
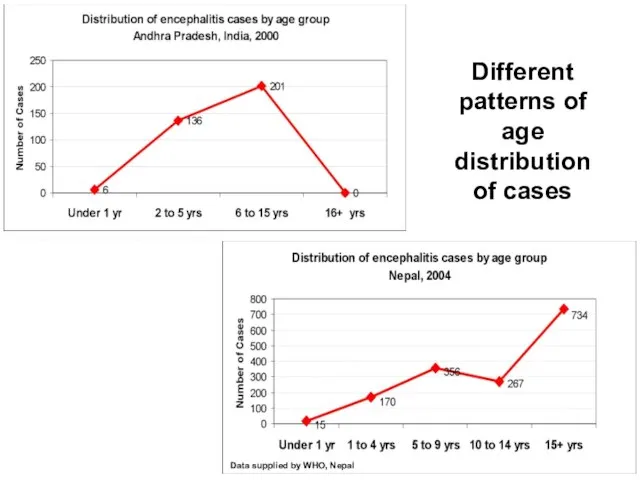
- 17. Age groups affected by JE Children 1 to 15 years of age are mainly affected in
- 18. Data supplied by Government of Andhra Pradesh Data supplied by WHO, Nepal Different patterns of age
- 19. Diagnosis and Treatment Laboratory diagnosis required Tentative diagnosis Antibody titer: HI, IFA, ELISA JE-specific IgM in
- 20. Vaccination Live attenuated vaccine horses and swine Successful for reducing incidence Inactivated vaccine (JE-VAX) Humans Japan,
- 22. Скачать презентацию
 Логистический аудит. Оценка качества, издержек и рисков. Модуль 1
Логистический аудит. Оценка качества, издержек и рисков. Модуль 1 Сахарный диабет. Лечение
Сахарный диабет. Лечение Вирус Иммунодефицита Человека
Вирус Иммунодефицита Человека Маскированная депрессия
Маскированная депрессия Дифференциальная диагностика пароксизмальных состояний
Дифференциальная диагностика пароксизмальных состояний Промышленные яды и их классификация. Показатели токсичности. Общие закономерности действия и направления профилактики
Промышленные яды и их классификация. Показатели токсичности. Общие закономерности действия и направления профилактики Двигательная функция и ее расстройства. Синдромы нарушения произвольных движений (параличи, парезы)
Двигательная функция и ее расстройства. Синдромы нарушения произвольных движений (параличи, парезы) Принципы антигипертензивной терапии
Принципы антигипертензивной терапии Временные пломбировочные материалы
Временные пломбировочные материалы МРТ голеностопного сустава и стопы 2012г
МРТ голеностопного сустава и стопы 2012г Идиопатические воспалительные миопатии: клиника, диагностика и лечение
Идиопатические воспалительные миопатии: клиника, диагностика и лечение Наследственные болезни человека
Наследственные болезни человека Сестринский уход за пациентами с заболеваниями носа и придаточных пазух
Сестринский уход за пациентами с заболеваниями носа и придаточных пазух Основы реабилитации: Инфракрасное излучение
Основы реабилитации: Инфракрасное излучение Особенности организации и оказания помощи пострадавшим с поражением ЧЛО на этапах медицинской эвакуации
Особенности организации и оказания помощи пострадавшим с поражением ЧЛО на этапах медицинской эвакуации Клинический случай
Клинический случай Метод контрольных вопросов
Метод контрольных вопросов Социально-биологические основы физической культуры
Социально-биологические основы физической культуры Хроническая обструктивная болезнь легких
Хроническая обструктивная болезнь легких Сахарный диабет у детей. Занятие 8
Сахарный диабет у детей. Занятие 8 Разбор препаратов
Разбор препаратов Тренировка замещения агрессии (ART)
Тренировка замещения агрессии (ART)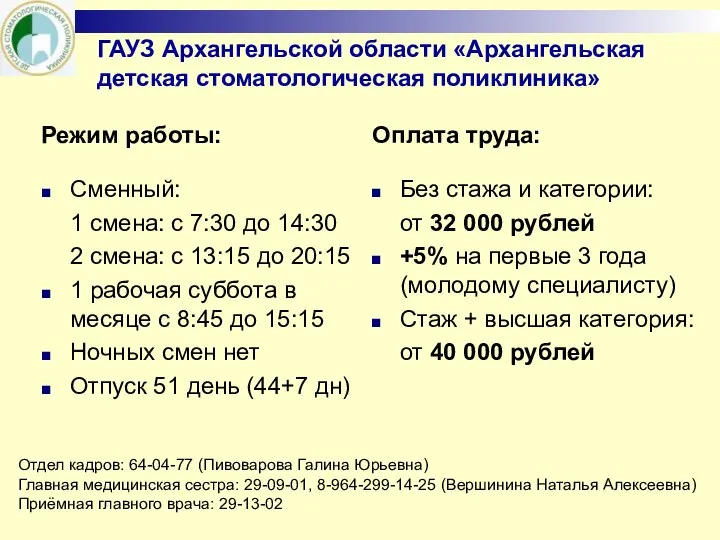 ГАУЗ Архангельской области Архангельская детская стоматологическая поликлиника
ГАУЗ Архангельской области Архангельская детская стоматологическая поликлиника Бесплодный брак
Бесплодный брак Продукты, получаемые из разных видов акул
Продукты, получаемые из разных видов акул Группы населения, подлежащие плановым прививкам
Группы населения, подлежащие плановым прививкам Развитие малой группы
Развитие малой группы Аутовоспалительные заболевания. Болезнь Бехчета/PFAPA синдром
Аутовоспалительные заболевания. Болезнь Бехчета/PFAPA синдром